Original Research
Traumatic Hip Dislocations in the Pediatric Patient: Injury Patterns, Need for Axial Imaging, Outcomes, and Selective Hip Arthroscopy
Children’s Healthcare of Atlanta, Atlanta, GA
Correspondence: Crystal A. Perkins, MD, Children’s Healthcare of Atlanta, 5445 Meridian Mark Rd., Suite 250, Atlanta, GA 30342. E-mail: [email protected]
Received: January 9, 2022; Accepted: March 10, 2022; Published: May 1, 2022
DOI: DOI: 10.55275/JPOSNA-2022-0034
Volume 4, Number 2, May 2022
Abstract:
Background: Traumatic hip dislocations are uncommon injuries in the pediatric population. Injury recognition and prompt closed reduction is standard of care. The purpose of this study is to describe injury patterns, treatment (including hip arthroscopy), and patient-reported outcomes of traumatic hip dislocation in pediatric patients.
Methods: A retrospective review was performed of all patients less than 18 years of age treated for a traumatic hip dislocation between 2011-2017 at a single center. Chart and radiographic review were performed, and patients were contacted to obtain outcome scores, including the Harris Hip score (HHS) and Hip Outcome Score (HOS).
Results: Twenty-three patients, 18 males and five females, with a mean age of 11.3 years (range 4-16) were included. The most common mechanisms of injury were motor vehicle crashes (8), football (7), and falls (3). The direction of hip dislocation was posterior (21) and obturator (2).
Twenty patients had a CT to assess the hip reduction and associated injuries and 15 (75%) had a posterior wall acetabular fracture and 6 (30%) had an incarcerated fragment within the joint. Five patients had an MRI and all had an associated posterior wall fracture and posterior labral tear.
Fourteen patients were treated nonoperatively. Patient-reported outcome scores were obtained in 10 patients (71%). Mean HOS-ADL, HOS-Sport, and mHHS were 75 (69–76), 32 (18-6), and 97 (85-100), respectively, at a mean of 40 months after injury.
Nine patients were treated operatively, including five patients with hip arthroscopy. Patient-reported outcome scores were obtained in seven patients (78%). Mean HOS-ADL, HOS-Sport, and mHHS were 69 (50-76), 30 (14-36), and 86 (59-100), respectively, at a mean of 34 months after surgery.
Conclusion: Traumatic hip dislocations in the pediatric population occur most frequently as isolated orthopaedic injuries in association with posterior wall acetabular fractures. Incarcerated fragments occurred in 30% of the patients yet were commonly not recognized on plain radiographs alone. Axial imaging should be routinely obtained following reduction. Selective hip arthroscopy after traumatic hip dislocations is a viable, less invasive method for treatment of incarcerated fragments and labral injury.
Level of Evidence: Level IV
Key Concepts:
- Pediatric and adolescent traumatic hip dislocations are rare and most often occur as an isolated orthopaedic injury.
- Advanced axial imaging should be obtained after reduction in all patients to evaluate for intraarticular pathology.
- Without incarcerated fragments, patients may be treated nonoperatively with good mid-term functional outcome scores.
- Selective hip arthroscopy may be effectively utilized in patients with intraarticular blocks to reduction and significant labral pathology as assessed on MRI.
Introduction
Traumatic hip dislocations are uncommon injuries in the pediatric population that typically result from high energy sports injuries or motor vehicle collisions. The femoral head may dislocate anteriorly, posteriorly, or into the obturator foramen and the direction of displacement dictates associated injury patterns. Upon recognition of the dislocation, prompt closed reduction is the standard of care. Prolonged time to reduction is associated with increased rates of osteonecrosis.1 Following closed reduction, radiographs must be carefully assessed to evaluate for a concentric reduction and associated injuries. Historically, a nonconcentric joint on radiographs has been an indication for further imaging with computerized tomography (CT) or magnetic resonance imaging (MRI).2 More recently, MRI has been advocated in the evaluation of many traumatic hip dislocations, as up to 25% of pediatric patients may have an interposed labrum or osteochondral fracture necessitating surgical intervention.3
The majority of patients can be treated nonoperatively following closed reduction. However, certain imaging findings or persistent hip pain may indicate intraarticular pathology that warrants surgical intervention. Intraarticular pathology has been described to include chondral injury, labral tears, osteochondral loose bodies, ligamentum teres injuries, and capsular tears.4 Indications for early surgical intervention following hip dislocations include an irreducible dislocation, joint incongruence with an incarcerated fragment, and a large acetabular fracture resulting in joint instability. Both open and arthroscopic approaches have been described following traumatic hip dislocations. Regardless of treatment type, traumatic hip dislocations have the potential for a myriad of complications including osteonecrosis, recurrent dislocation, posttraumatic osteoarthritis, neurologic injury, coxa magna, and heterotopic ossification. Despite these risks, hip arthroscopy has been shown to be a safe and effective treatment option for select patients.
The purpose of this study was to describe a series of traumatic hip dislocations in pediatric patients, including injury patterns, imaging findings, and nonoperative and operative treatment. Secondarily, we sought to describe patient-reported outcomes at 12-months follow-up. We hypothesized that plain radiographs frequently miss posterior wall fractures and incarcerated fragments which are otherwise detected by advanced axial imaging.
Methods
After Institutional Review Board (IRB) approval, a single institution retrospective review of patients less than 19 years of age treated for a traumatic hip dislocation between 2011-2017 was performed. The initial patient cohort was compiled by querying the electronic medical record and physician billing records using Current Procedural Code (CPT) 27250 (closed treatment of hip dislocation, traumatic, without anesthesia), 27252 (closed treatment of hip dislocation, traumatic, with anesthesia), 27253 (open treatment of hip dislocation, traumatic, without internal fixation), 27254 (open treatment of hip dislocation, traumatic, with acetabular and femoral head fracture), International Classification of Disease (ICD)-9 code 835.00 (closed dislocation of hip) and ICD-10 code S73.0 (subluxation and dislocation of hip). Inclusion criteria was age <19 years old and a traumatic hip dislocation. Patients with nontraumatic hip dislocations (developmental hip dysplasia or neuromuscular etiology) were excluded. Demographic information (age, sex, BMI, mechanism of injury), treatment details, and clinical outcomes were obtained via chart review. Avascular necrosis and chondrolysis were defined as complications.
Imaging
Injury radiographs were assessed to determine the direction of the dislocation. Immediate postreduction radiographs as well as applicable advanced imaging (CT or MRI) were reviewed for the presence of a concentric reduction, intraarticular injury, or other concomitant injury. The decision to order a postreduction CT or MRI was determined by surgeon preference. Final clinical follow-up radiographs were reviewed for the development of avascular necrosis and chondrolysis.
Patient-Reported Outcomes
All patients were attempted to be contacted via phone, email, or at their most recent clinical visit to complete two validated hip specific outcome measures: modified Harris Hip Score (mHHS) and Hip Outcome Score (HOS). The modified Harris Hip Score is a 91 point questionnaire evaluating pain, function, range of motion, and deformity.5 The score is multiplied by 1.1 to give a maximum total score of 100. The Hip Outcome Score evaluates for limitations in both activities of daily living (ADLs) and sports due to patient’s hip symptoms.6 There are 19 questions with a maximum potential score of 68 points for the ADL subsection and nine questions for maximal score of 36 in the sports subsection. If patients were unable to be contacted for collection of PROs and clinical follow-up was less than 12 months, then those patients were excluded for the purposes of analyzing outcomes.
Statistical Analysis
Statistical analyses were performed using SAS 9.3 (Cary, NC, 2002-2010). Descriptive statistics were calculated for study population characteristics, including means and standard deviations for continuous variables and frequencies and percentages for dichotomous or categorical variables. Two-sample t-tests were performed for continuous variables. P-values were generated and statistical significance was assessed at the 0.05 level.
Results
Twenty-three patients, including 18 males and 5 females, with a mean age of 11.3 years (range 4-16) were included. Proximal femoral physes were open in 21 patients (91%) and closed in 2 patients (9%). Triradiate cartilages were open in 15 patients (65%) and closed in 8 patients (35%). The most common mechanisms of injury were motor vehicle crashes (MVC) (n=8), football (n=7), and falls (n=3). The direction of hip dislocation was posterior (n=21, 91%) and obturator (n=2, 9%). All were closed injuries and there were no associated neurovascular injuries. The majority of patients (87%) had isolated orthopaedic injuries. Secondary orthopaedic injuries were seen in two patients: a 7-year-old male s/p MVC with an obturator hip dislocation and an ipsilateral subtrochanteric femur fracture (Figure 1), and an 8-year-old male s/p MVC with an ipsilateral distal fibula fracture. Three patients (13%) had nonorthopaedic injuries, all of which were closed head injuries.
Figure 1. 8-year-old male status post motor vehicle collision with left obturator hip dislocation and ipsilateral subtrochanteric femur fracture (a). This was treated with closed reduction of the hip in the operating room followed by flexible intramedullary nail fixation of the femur (b).

Five patients had spontaneous reduction of the hip dislocation prior to arrival, all of whom had CT imaging consistent with hip dislocation (posterior soft tissue injury and hip effusion) with a posterior wall acetabular fracture in all patients. Of the remaining 18 patients, 15 (83%) had closed reduction performed with procedural sedation in the emergency department at a mean of 2.6 hours (range 1–5 hours) following the time of injury. Three patients (17%) were taken to the operating room for closed reduction, including the patient in Figure 1 with an ipsilateral subtrochanteric femur fracture and a 16-year-old male with a large posterior wall fracture treated with closed reduction and distal femoral traction pin placement. A third patient, an 8-year-old male with a closed head injury and diffuse axonal injury s/p MVC, was transferred to our facility for inpatient rehab 15 days following his initial injury. On tertiary exam, he was noted to have pain with hip motion, and radiographs performed at that time identified a posterior hip dislocation. Given the chronicity of his injury, he was taken to the operating room for closed reduction, arthrogram, and spica cast application.
Imaging
All who presented with the hip dislocated had a prereduction anterior-posterior (AP) pelvis radiograph, and all patients had an AP pelvis radiograph with the hip in a reduced position. In addition, 20 patients had an immediate postreduction CT to assess the joint congruence and associated injuries. Fifteen of those patients (75%) had a posterior wall acetabular fracture and six (30%) had an incarcerated fragment within the joint visible on CT. Five patients, including the three patients without a CT and two patients with a CT, had a postreduction hip MRI and all had an associated posterior wall fracture and posterior labral tear. The corresponding CT and MRI images of the two patients with both imaging modalities are depicted in Figure 2.
Figure 2. Postreduction axial CT (a) and MRI (b) illustrating posterior wall acetabular fracture with incarcerated intraarticular osteochondral loose body.
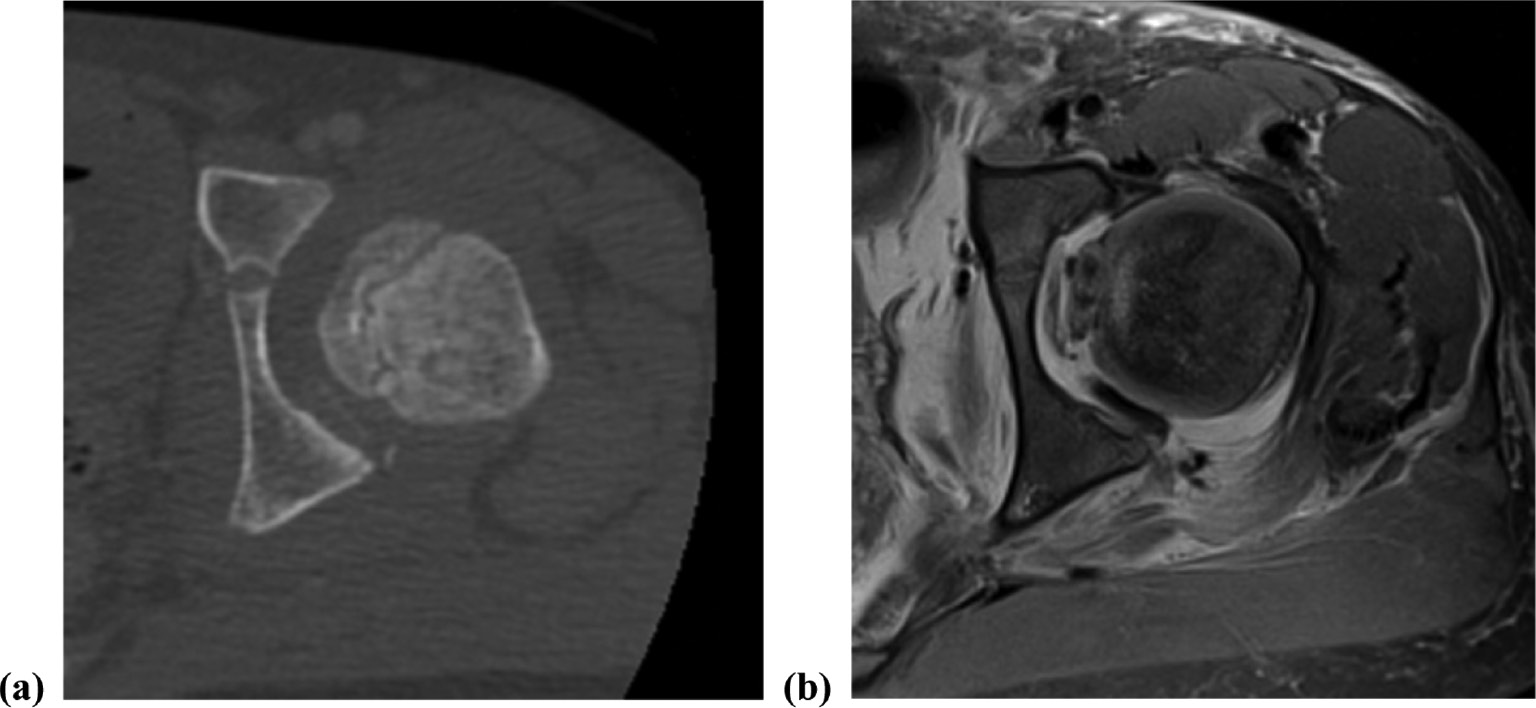
Of the 20 patients with a posterior wall fracture on advanced imaging, only five (25%) had a fracture visible on postreduction radiographs. Of the five patients with an incarcerated fragment identified on advanced imaging, only two (40%) had a nonconcentric reduction on postreduction radiographs. Patients with a posterior wall fracture were older (mean age 12.5 years) as compared to those without a posterior wall fracture (mean age 8.5 years), p=0.002.
Nonoperative Management
Fourteen patients (61%) were treated nonoperatively and are listed in Table 1. The mean age of nonoperatively treated patients was 11.1 years (range 4-16 years). Nonoperative treatment included protected weight bearing for 3-6 weeks and posterior hip precautions in all patients. An abduction pillow and/or knee immobilizer was used in 10 patients. Eleven of 14 patients had minimum 12-month clinical or PRO follow-up (median 37 months, range 20-83 months).
Table 1. List of Nonoperative Patients
| Sex | Age | Laterality | Mechanism | Dislocation | Associated Injuries | Time from Injury to Reduction | Follow-up Duration (months) | Complications |
|---|---|---|---|---|---|---|---|---|
| M | 4 | L | Fall | Posterior | 3 hours | 0* | ||
| M | 8 | L | MVC | Posterior | PW fx | 2 hours | 83 | AVN without collapse |
| M | 8 | R | MVC | Posterior | 3 hours | 25 | ||
| M | 9 | L | Football | Posterior | Spontaneous | 42 | ||
| M | 10 | R | Football | Posterior | PW fx | 3 hours | 55 | |
| M | 10 | R | MVC | Posterior | 1 hour | 24 | ||
| M | 11 | L | Football | Posterior | PW fx | 2 hours | 2* | |
| M | 11 | R | Football | Posterior | 2 hours | 79 | ||
| F | 11 | L | Fall | Obturator | 1 hour | 10* | ||
| M | 12 | R | Football | Posterior | PW fx | 3 hours | 26 | |
| F | 12 | R | Soccer | Posterior | PW fx | 3 hours | 56 | |
| M | 12 | L | Football | Posterior | 5 hours | 20 | ||
| M | 14 | L | Dirtbike | Posterior | PW fx | Spontaneous | 22 | |
| F | 16 | L | MVC | Posterior | PW fx | 2 hours | 37 |
MVC = motor vehicle collision, PW fx = posterior wall fracture
* Not included in analysis of outcomes
Follow-up radiographs were normal in all except one patient. An 8-year-old male, with closed reduction of a posterior hip dislocation 2 hours following injury, was noted to have a crescent sign on radiographs at 6 months following his injury and MRI demonstrated avascular necrosis without collapse (Figure 3). No further follow-up was able to be obtained on this patient. Patient-reported outcome scores were obtained in 10 of the 11 patients with minimum 12-month follow-up at a median of 40 months (range 20-83 months). Median HOS-ADL, HOS-Sport, and HHS were 76 (69-76), 36 (18-36), and 91 (85-100), respectively, at a mean of 40 months (20-83 months) after injury.
Figure 3. 8-year-old male s/p MVC with left hip dislocation who developed a crescent sign on plain radiographs (a) and AVN without collapse on MRI (b) 6 months following closed reduction and nonoperative treatment.

Operative Management
Nine patients (39%) were treated operatively, including five patients with hip arthroscopy, and they are listed in Table 2. The remaining four operative cases were treated with an exam under anesthesia and A-frame casting, arthrogram and spica cast, closed reduction and distal femoral traction pin placement on the date of presentation and open reduction internal fixation of a large posterior wall acetabular fracture 2 days later, and closed reduction and flexible intramedullary nailing of the femur in a patient with an ipsilateral subtrochanteric femur fracture. No patient was treated with surgical hip dislocation. The mean age of operatively treated patients was 11.5 years (range 7-15 years).
Table 2. List of Operatively Treated Patients
| Sex | Age | Laterality | Mechanism | Dislocation | Associated Injuries | Time from Injury to Reduction | Surgical Treatment | Follow-up Duration (months) | Complications |
|---|---|---|---|---|---|---|---|---|---|
| M | 7 | L | Kicked bookshelf | Posterior | 10 days | EUA, A-frame cast | 63 | ||
| M | 7 | L | MVC | Obturator | Subtrochanteric femur fracture | 4 hours | Closed reduction, ORIF femur | 49 | |
| M | 8 | R | MVC | Posterior | PW fx, posterior labral tear, SDH, DAI | 16 days | EUA, closed reduction, arthrogram, spica cast | 20 | |
| M | 10 | L | MVC | Posterior | PW fx | Spontaneous | Hip scope, reduction of entrapped labrum | 46 | |
| F | 10 | R | Fall | Posterior | PW fx, incarcerated fragment | Spontaneous | Hip scope, LBR | 2* | |
| M | 13 | R | Football | Posterior | PW fx, incarcerated fragment | 1 hour | Hip scope, LBR, chondroplasty acetabulum, posterior labral repair | 43 | Anterior head-neck junction exostosis causing anterior impingement |
| M | 14 | R | MVC | Posterior | PW fx | 4 hours | Hip scope, anterior and posterior labral repair, loose body removal, microfracture acetabulum | 20 | Chondrolysis |
| F | 15 | L | MVC | Posterior | PW fx, incarcerated fragment, posterior labral tear | Spontaneous | Hip scope, LBR, posterior labral repair, microfracture acetabulum | 13 | |
| M | 16 | R | Basketball | Posterior | PW fx | 12 hours | ORIF acetabulum | 0* |
EUA = exam under anesthesia, LBR = loose body removal
* Not included in analysis of outcomes
The indication for hip arthroscopy was an incarcerated fragment in four patients and an entrapped labrum with incongruent reduction in one patient. Arthroscopic procedures included loose body removal, labral repair, and acetabular microfracture in two patients, loose body removal and labral repair in one patient, and reduction of the entrapped labrum with debridement of the ligamentum teres in one patient. Mean operative time for arthroscopic cases was 105 minutes (range 80-134 minutes). Figure 4 demonstrates an intraarticular loose body and posterior labral repair. One operatively treated patient was from out-of-state and returned home for all clinical and radiographic follow-up. Among the other eight patients, mean clinical and radiographic follow-up was 16 months (range 2-36 months).
Figure 4. Intraoperative arthroscopy illustrating large chondral intraarticular loose body (a) and posterior labral repair (b).

One patient, a skeletally immature 14-year-old male, developed joint space narrowing and chondrolysis following hip arthroscopy. His clinical course is depicted in Figure 5. This patient sustained a posterior hip dislocation as a result of an MVC and underwent a successful single attempt closed reduction under sedation 4 hours following time of injury. Postreduction radiographs revealed a nonconcentric reduction and CT demonstrated a posterior wall acetabular fracture with intraarticular chondral fragment. On post-injury day 1, he underwent exam under anesthesia, hip arthroscopy, anterior and posterior labral repair, chondral loose body removal (12 mm × 6 mm), and microfracture of the anterior acetabulum. The loose body was a full-thickness chondral injury of the anterior acetabulum at the 2-3 o’clock position. Postoperatively, he was treated with protected weight-bearing for 8 weeks, an abduction pillow, and posterior hip precautions. Physical therapy was initiated at 2 weeks postoperative for gentle hip range of motion. At 6 months postoperatively, he was noted to have joint space narrowing on radiographs and a decline in his hip motion. Inflammatory labs were normal and MRI was consistent with chondrolysis and no evidence for infection. He had transient improvement in symptoms with an intraarticular corticosteroid injection, but ultimately, he had progressive joint space narrowing, limited and painful motion, and was referred for hip arthroplasty 21 months post-injury.
Figure 5. 14-year-old male s/p MVC with right posterior hip dislocation (a). This was treated with prompt closed reduction in the emergency room with sedation (b) and subsequent hip arthroscopy with loose body removal, microfracture of the acetabulum, and posterior labral repair. A well-reduced concentric joint is noted at 2 weeks postop (c). At 6 months postop (d), there has been concentric joint space narrowing consistent with chondrolysis. At 20 months postop (e), there is significant pelvic tilt and progressive near complete joint space loss with coxa profunda.

A second patient, a 13-year-old male s/p posterior hip dislocation as a result of a football injury underwent hip arthroscopy, loose body removal, and posterior labral repair. Postoperatively, he was noted to develop an exostosis along the anterior head-neck junction and symptomatic CAM impingement (Figure 6). This was felt to have developed as a result of ossification of a periosteal avulsion at the time of initial injury and ultimately required hip arthroscopy, anterior labral repair, and femoroplasty 29 months after his initial injury. At 36-month follow-up, he was asymptomatic and had returned to high school football and, ultimately, collegiate football.
Figure 6. 13-year-old male s/p right hip dislocation playing football. He was initially treated with hip arthroscopy, loose body removal, chondroplasty of the posterior acetabulum, and posterior labral repair. At 9 months postoperatively, he was noted to have an exostosis along the anterior head-neck junction (a). At 14 months postoperatively, he had symptomatic CAM impingement (b). Twenty-nine months following his initial injury, he underwent revision hip arthroscopy, lysis of adhesions, femoroplasty, and anterior labral repair (c).

Seven of the nine operatively treated patients (78%), including four of five (80%) hip arthroscopy patients, had minimum 12-month follow-up (median 43 months, range 13-63 months) and all had PROs. One patient’s reported outcomes were significantly inferior secondary to his severe closed head injury (HOS-ADL 50, HOS-Sport 14, HHS 59). The second clear outlier was the patient who developed chondrolysis (HOS-ADL 63, HOS-Sport 23, HHS 75). Median HOS-ADL, HOS-Sport, and HHS among the remaining five patients were 74 (69-76), 36 (32-36), and 91 (67-100), respectively, at a mean of 43 months (13-63) after surgery. Inclusive of all patients, there were no significant differences in mean patient-reported outcome measures between nonoperative and operative cohorts; HOS-ADL 75 v 69 (p=0.08), HOS-Sport 32 v 30 (p=0.60), HHS 97 v 86 (p=0.07).
Discussion
In this series of 23 pediatric traumatic hip dislocations, most occurred as a result of high energy mechanisms (MVC 39%, football 30%), and postreduction advanced imaging demonstrated posterior wall acetabular fractures in 78% and incarcerated fragments in 30% of patients. Overall, both nonoperative and operative treatment of these injuries was associated with good to excellent patient-reported outcome measures at median 40- and 43-month follow-up, respectively. Selective hip arthroscopy for the treatment of loose bodies and labral pathology following traumatic hip dislocation was associated with excellent patient-reported outcomes in most cases. Avascular necrosis occurred in one patient (4%) with nonoperative treatment and chondrolysis in one patient (4%) with operative treatment.
The most important initial step following diagnosis of a traumatic hip dislocation is prompt closed reduction. Mehlman et al. evaluated 42 skeletally immature patients with a traumatic hip dislocation and noted a 20 times higher risk of AVN if reduction was delayed greater than 6 hours.1 While urgent reduction is necessary, the authors note it is equally as vital for reduction to be done with appropriate sedation and technique in a controlled setting. Extra care should be taken in adolescent patients to detect physeal instability prior to formal reduction to minimize the risk of traumatic epiphysiolysis, which uniformly has poor outcomes associated with the development of AVN.7–9 The literature reports the incidence of this to be 2.3% in pediatric traumatic hip dislocations,10 yet no patients in our series had this complication. In skeletally immature patients with high-energy injury mechanisms and concern for physeal instability, hip reduction can be performed with live fluoroscopy to detect physeal instability prior to complete epiphysiolysis.9
Postreduction imaging must be scrutinized closely for any joint asymmetry which could represent entrapped bone or soft tissue in the joint. Furthermore, postreduction advanced axial imaging should be performed routinely. In our series, posterior wall acetabular fractures and incarcerated fragments were not visualized on plain radiographs in 75% and 40% of cases, respectively. Although additional radiographs, such as Judet views, may have demonstrated the posterior wall fractures, they would not have captured the cartilaginous injuries, incarcerated fragments, and labral injury. Additionally, many patients had a CT completed as part of their trauma workup prior to orthopaedic consultation. The standard of care in adult patients is to obtain a postreduction CT; however, this may not be sufficient in the pediatric population.11,12 As noted in our study, the average age of patients with a posterior wall fracture was older than those without, likely secondary to the fact that younger children do not yet have ossification of the posterior wall of the acetabulum. Due to the delay in the posterior wall ossification and potential to miss cartilaginous fractures or other soft tissue entrapment, other authors have recommended the use of MRI instead of CT to more accurately evaluate hip pathology in pediatric patients with an open triradiate cartilage.13,14 All five patients in our study with postreduction MRI had associated posterior wall fractures and labral tears compared to CT detection of this pathology in 75% of our patients.
It should be noted that the clinical significance of small posterior wall acetabular fractures following traumatic hip dislocations in pediatric patients is not well-established. In our series, only one of these injuries, a 6 cm posterior wall fracture in a 16-year-old patient, required operative treatment specifically for the fracture. Given the young age of our cohort, (mean age 11 years) with 74% of the cohort 12 years or younger, and the fact that the secondary ossification center in the posterior acetabulum rim appears at age 12 years in females and 14 years in males15, clinically significant posterior wall fractures were not identified.
If intraarticular pathology is confirmed as the source of a non-concentric reduction, surgical intervention is recommended. Traditionally, this was performed through open3,16,17 surgical approaches, but advancements in arthroscopic4,18–20 techniques have made it a viable option that is substantially less invasive. Vialle et al. reported on 35 traumatic dislocations in skeletally immature patients with nine requiring surgery to achieve an anatomic reduction.3 All surgeries were performed through an open anterior arthrotomy with removal of an osteochondral fragment. While the osteochondral fragments could be visualized and removed through this approach, they could not be repaired. Two patients in their series developed AVN, though these patients each had delayed reductions >10 hours following the time of injury. Podeszwa et al. reviewed 11 male patients, mean age 12.3 years treated with a surgical hip dislocation (SHD) to manage intraarticular pathology following a traumatic hip dislocation.16 The most common intraoperative findings included labral tears (n=8), femoral head chondral injuries (n=5), and acetabular rim fractures (n=4). The authors reported one transient postoperative peroneal nerve palsy but no radiographic evidence of avascular necrosis at mean 24-month follow-up. The mean HHS at 1 year was 95 (84-100). Novais et al. reported similar successful results among eight patients undergoing SHD with posterior capsule and labral repair.17 Eighty-eight percent of their patients reported maximum HHS with no cases of avascular necrosis. While both studies highlight successful outcomes and a technique that allows direct visualization and repair, a SHD remains an invasive and technically demanding operation.
Hip arthroscopy, while also technically demanding, offers a less invasive technique to diagnose and treat chondral, labral, and capsular injuries following traumatic hip dislocation. The senior author’s experience is that hip arthroscopy after a recent dislocation does not create additional difficulties with visualization despite the capsule being torn in all cases. Several precautions should be taken, however. Acutely after a hip dislocation, hip distraction can be performed with less traction forces than typical, so fluoroscopy should be used to evaluate for adequate distraction. The distraction force is often able to be decreased after initial distraction while maintaining adequate distraction. Difficulty due to fluid extravasation was not encountered although time must be taken initially to lavage the joint to remove the traumatic hematoma. Lastly, fluid pump pressures should be maintained as low as possible, typically 35-40 mmHg, to avoid unnecessary fluid use.
Phillipon et al. described the findings of 14 elite athletes who underwent hip arthroscopy after traumatic dislocation and noted all patients to have labral tears and femoral chondral lesions.4 Ilizaliturri et al. and Yamamoto et al. each noted a similar incidence of chondral and labral pathology along with high percentages of intraarticular loose bodies in their patients undergoing hip arthroscopy after dislocation.18,21 Outcomes in adult patients, as described in a systematic review by Mandell et al., are excellent with 84% of patients having no residual functional limitation, pain or osteoarthritis at final follow-up after hip arthroscopy for management after a traumatic hip dislocation. Seventy-five of the 151 included patients were followed for a median of 2 years postoperatively, with osteoarthritis reported in 4% and avascular necrosis in 2.7%.22
Hip arthroscopy has been shown to be safe and successful in treating a variety of pediatric hip conditions.23 Specific to the treatment of traumatic hip dislocations, Wylie et al. evaluated 12 patients with a mean age of 16 years (range 11-25) who underwent hip arthroscopy.19 Similar to studies of adults, the authors noted 83% of patients to have a loose body, labral injury, or chondral injury. This, however, was a mixed adult and pediatric population and described only imaging and arthroscopic findings and not clinical outcomes. Morris et al. reviewed seven pediatric patients treated with hip arthroscopy after traumatic hip dislocation and noted that 71% of patients had an enfolded avulsion of the posterior capsular-labral soft tissue complex which was blocking concentric reduction.20 This is similar to our study which identified 80% of patients undergoing hip arthroscopy to have damage to the posterior labrum. No avascular necrosis or instability was noted in their cohort, but average follow-up was only 10 months and patient-reported outcome scores were available in only two patients.
Chondrolysis with rapid progressive loss of joint space on radiographs and clinical loss of hip motion has been described as a result of several etiologies: thermal, chemical, infection, mechanical (surgical insult or prominent hardware), or traumatic joint injury. Surgical factors can include vascular injury (medial femoral circumflex artery), iatrogenic chondral injury, and high intracapsular pressure. In the patient in this series who developed chondrolysis, the circumflex arteries were visualized without evidence for arthroscopic injury, there were no iatrogenic chondral injuries, and a pressure- and flow-controlled pump was used throughout the procedure to maintain pressure within a 35-45 mm Hg range. We confirmed the absence of postoperative infection based on normal inflammatory labs and a negative intraarticular synovial fluid culture. Although a surgical etiology of the chondrolysis cannot be 100% confirmed, we feel strongly that the chondrolysis most likely occurred as a result of the initial traumatic injury.
Our study is not without limitations. The study is retrospective in nature, and treatment was not randomized but directed at the discretion of the attending surgeon managing the patient. There may be a selection bias in terms of injury severity and nonoperative and operative treatment decisions; thus, the study was not designed to compare treatment groups. The sample size is relatively small, though this is not unexpected given the rare nature of pediatric traumatic hip dislocations, particularly those requiring surgical intervention. Two patients were from out-of-state, clinical and radiographic follow-up is not available, and these patients did not respond to attempts to achieve patient-reported outcome measures. Although longer-term follow-up will be beneficial for description of mid- and long-term outcomes, the intent of this study was to describe injury patterns, imaging findings, and treatment types. For the purposes of describing outcomes, we included only those patients who had minimum 12-month follow-up, which was 78% our cohort. Patient-reported outcome measures were obtained in 74% of patients at a median of 40 months among nonoperative patients and 43 months among operative patients. However, the lack of PROs on all patients may result in bias and overestimation of the positive outcomes. However, among pediatric patients, this is the largest collection of patient-reported outcomes measures following traumatic hip dislocation. Lastly, the PROs utilized in this study, HHS and HOS, have not been formally validated in the pediatric population. Despite this, they are the most widely used outcomes scores in this population. Although the Children’s Hospital Oakland Hip Evaluation Scale (CHOHES) has been validated in pediatric patients, its use is currently rare. For that reason, HHS and HOS were utilized as they are most familiar to readers.
Conclusion
Pediatric and adolescent traumatic hip dislocations are rare and most often occur as an isolated orthopaedic injury. Prompt reduction under appropriate conditions is vital as is critical review of postreduction radiographs. Advanced axial imaging, preferably an MRI, should be obtained after reduction in all patients to evaluate for intraarticular pathology. Without incarcerated fragments, patients may be treated nonoperatively with good mid-term functional outcome scores, while selective hip arthroscopy may be effectively utilized in patients with intraarticular blocks to reduction and significant labral pathology.
Disclaimer
No funding was received for this study. S. Willimon: Consultant for Smith & Nephew and Vericel; A. Egger and C. Perkins have no conflicts of interest to report.
References
- Mehlman CT, Hubbard GW, Crawford AH, et al. Traumatic hip dislocation in children. Long-term followup of 42 patients. Clin Orthop Relat Res. 2000;(376):68-79.
- Price CT, Pyevich MT, Knapp DR, et al. Traumatic hip dislocation with spontaneous incomplete reduction: a diagnostic trap. J Orthop Trauma. 2002;16(10):730–735.
- Vialle R, Odent T, Pannier S, et al. Traumatic hip dislocation in childhood. J Pediatr Orthop. 2005;25(2):138-144.
- Philippon MJ, Kuppersmith DA, Wolff AB, et al. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25(2):169-174.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755.
- Martin RL, Philippon MJ. Evidence of validity for the hip outcome score in hip arthroscopy. Arthroscopy. 2007;23(8):822-826.
- Barquet A, Vecsei V. Traumatic dislocation of the hip with separation of the proximal femoral epiphysis. Report of two cases and review of the literature. Arch Orthop Trauma Surg. 1984;103(3):219-223.
- Fiddian NJ, Grace DL. Traumatic dislocation of the hip in adolescence with separation of the capital epiphysis. Two case reports. J Bone Joint Surg Br. 1983;65(2):148-149.
- Herrera-Soto JA, Price CT, Reuss BL, et al. Proximal femoral epiphysiolysis during reduction of hip dislocation in adolescents. J Pediatr Orthop. 2006;26(3):371-374.
- Herrera-Soto JA, Price CT. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg. 2009;17(1):15-21.
- Rubel IF, Kloen P, Potter HG, et al. MRI assessment of the posterior acetabular wall fracture in traumatic dislocation of the hip in children. Pediatr Radiol. 2002;32(6):435-439.
- Hearty T, Swaroop VT, Gourineni P, et al. Standard radiographs and computed tomographic scan underestimating pediatric acetabular fracture after traumatic hip dislocation: report of 2 cases. J Orthop Trauma. 2011;25(7):e68-e73.
- Fabricant PD, Hirsch BP, Holmes I, et al. A radiographic study of the ossification of the posterior wall of the acetabulum: implications for the diagnosis of pediatric and adolescent hip disorders. J Bone Joint Surg Am. 2013;95(3):230-236.
- Thanacharoenpanich S, Bixby S, Breen MA, et al. MRI is better than CT scan for detection of structural pathologies after traumatic posterior hip dislocations in children and adolescents. J Pediatr Orthop. 2020;40(2):86-92.
- Morris WZ, Chen JY, Cooperman DR, et al. Characterization of ossification of the posterior rim of acetabulum in the developing hip and its impact on the assessment of femoroacetabular impingement. J Bone Joint Surg Am. 2015;97(3):e11.
- Podeszwa DA, De La Rocha A, Larson AN, et al. Surgical hip dislocation is safe and effective following acute traumatic hip instability in the adolescent. J Pediatr Orthop. 2015;35(5):435-442.
- Novais EN, Heare TC, Hill MK, et al. Surgical hip dislocation for the treatment of intra-articular injuries and hip instability following traumatic posterior dislocation in children and adolescents. J Pediatr Orthop. 2016;36(7):673-679.
- Ilizaliturri VM, Jr., Gonzalez-Gutierrez B, Gonzalez-Ugalde H, et al. Hip arthroscopy after traumatic hip dislocation. Am J Sports Med. 2011;39 Suppl:50s-57s.
- Wylie JD, Abtahi AM, Beckmann JT, et al. Arthroscopic and imaging findings after traumatic hip dislocation in patients younger than 25 years of age. J Hip Preserv Surg. 2015;2(3):303-309.
- Morris AC, Yu JC, Gilbert SR. Arthroscopic treatment of traumatic hip dislocations in children and adolescents: a preliminary study. J Pediatr Orthop. 2017;37(7):435-439.
- Yamamoto Y, Ide T, Ono T, et al. Usefulness of arthroscopic surgery in hip trauma cases. Arthroscopy. 2003;19(3):269-273.
- Mandell JC, Marshall RA, Banffy MB, et al. Arthroscopy after traumatic hip dislocation: a systematic review of intra-articular findings, correlation with magnetic resonance imaging and computed tomography, treatments, and outcomes. Arthroscopy. 2018;34(3):917-927.
- Jayakumar P, Ramachandran M, Youm T, et al. Arthroscopy of the hip for paediatric and adolescent disorders: current concepts. J Bone Joint Surg Br. 2012;94(3):290-296.
