Original Research
Early Failure of Locking Compression Plates in Pediatric Proximal Femoral Fracture
1University of Tennessee-Campbell Clinic Department of Orthopaedic Surgery & Biomedical Engineering, Memphis, TN; 2University of Tennessee Health Science Center, College of Medicine, Memphis, TN; 3Le Bonheur Children’s Hospital, Memphis, TN
Correspondence: Derek M. Kelly, MD, Campbell Clinic Orthopaedics, 1211 Union Ave., Suite 510, Memphis, TN. E-mail: [email protected]
Received: February 16, 2023; Accepted: May 5, 2023; Published: August 1, 2023
Volume 5, Number 3, August 2023
Abstract
Background: Although proximal femoral locking compression plates (PF-LCP) have been used with increasing frequency in the fixation of proximal femoral fractures in the pediatric population, there is a lack of literature regarding their use. The purpose of this study was to examine the failure rates of PF-LCP fixation in comparison to other accepted fixation methods within a pediatric population.
Methods: Retrospective review identified consecutive children treated for proximal femoral fractures from September 2008 to February 2019, who had a minimum follow-up of 12 weeks. Patient charts and radiographs were reviewed, and demographic information was compiled. In the case of failures, timing and method of failure were documented.
Results: Sixty-four proximal femoral fractures (61 children) were studied. The average age at the time of presentation was 10.4 years. Twenty-six fractures were treated with PF-LCPs and 38 with other fixation methods (compression hip screws, rigid locked intramedullary nailing, cannulated screws, or a combination of hip screw side plate and intramedullary nailing). Failure occurred in four of the 26 fractures treated with locking compression plating (15.4%) compared to none of the 38 treated with other fixation types (p<0.05).
Conclusions: This study demonstrates a higher rate of failure in proximal femoral fractures, particularly basicervical and transcervical femoral neck fractures, treated with locking compression plates (12.9%) compared to 0% other fixation methods (no failures). As a result of this study, we no longer use locked plating systems for pediatric femoral neck fractures at our institution.
Level of Evidence: Level III
Key Concepts
- Proximal femoral fractures account for less than 1% of all fractures in children.
- Locking compression plates are being more frequently used in pediatric proximal femoral fractures.
- Outcome studies are limited because of the low incidence of these fractures and relative recent introduction of this fixation method.
- Proximal femoral compression locking plates had a higher rate of early mechanical failure than other fixation modalities in this study.
- The increased risk of failure with proximal femoral compression locking plates should be considered before opting for these implants.
Introduction
Pediatric proximal femoral fractures have an incidence of <1% of all fractures in children.1,2 They are a rare but serious injury with high risk of further complications and disability.3 Long-term complications include pain, osteonecrosis, coxa vara, proximal femoral physeal arrest, and nonunion. Complications are common, affecting up to 50% of patients. These fractures often result from high-energy trauma, such as a fall from height or motor vehicle collision and are often complicated by other injuries, such as head and facial trauma, splenic laceration, retroperitoneal hemorrhage, and perineal injury.3–5 Other musculoskeletal injuries are common as well, including pelvic ring and acetabular injuries, hip dislocation, and ipsilateral fractures of the femur.3
Treatment of pediatric proximal femoral fractures consists of anatomic reduction and stable fixation.6,7 Several different forms of instrumented stabilization are available for definitive fixation including smooth pins, cannulated screws, pediatric sliding hip screw, blade plate, intramedullary nail, and proximal femoral locking plate.3 All of these fixation methods have different indications based on fracture classification and patient age as well as surgeon training and preference.
Proximal femoral locking compression plates (PF-LCP) were introduced to facilitate intertrochanteric and subtrochanteric osteotomies, but their indications have been expanded to include fracture fixation of the proximal femur.5 Initial biomechanical studies were promising, showing increased strength over similar locked angle constructs, and led to the plate being used for fixation in both adults and children. Clinical studies, however, began to show challenges in this plate’s use in adults such as increased rate of complications compared to biomechanical studies and mechanical failure in unstable fractures.8,9 Proximal femoral fractures are more common in adults than in children, which may account for the literature providing evidence of outcomes in adults earlier than children.10 Studies of the use of PF-LCPs in the pediatric population have been limited by small sample sizes and by combining osteotomy and fracture patients in the same analysis.11,12 The paucity of literature regarding the use of the PF-LCPs in children is likely due to a combination of factors, including the relatively recent introduction of the plate itself and the low incidence of these fractures.
The goal of this study was to examine the use of proximal femoral locking compression plates in pediatric proximal femoral fractures and determine the frequency of implant failure in these patients. A better understanding of these fixation methods will add to the pediatric orthopaedic trauma literature and improve patient outcomes by helping surgeons choose the most reliable implants. We hypothesized that the PF-LCP would show a higher early mechanical failure rate than other forms of fixation in pediatric proximal femoral fractures.
Materials and Methods
After obtaining Institutional Review Board approval, an institutional database review identified 61 patients (64 fractures) who had fixation of proximal femoral fractures at our Level 1 pediatric trauma center between September 2008 and February 2019. All surgeries were performed by one of six fellowship-trained pediatric orthopaedic surgeons. The decision as to implant type was made based on fracture type, presence of comorbidities, and patient age along with surgeon experience and preference.
Inclusion criteria were age 18 years or younger at the time of injury, with a fracture of the proximal femoral region that could be appropriate for fixation with a PF-LCP, including femoral neck fractures, intertrochanteric fractures, and some subtrochanteric fractures. Fractures of this entire region of the proximal femur were chosen for study in order to capture as many injuries as possible because fractures of this area in the pediatric population are quite uncommon. Pathologic fractures were included. Exclusion criteria included age greater than 18 years. Femoral head fractures, slipped capital femoral epiphysis, and planned osteotomies were not included in record retrieval or analysis.
Demographics and patient information (Table 1), such as other medical conditions, mechanism of trauma, and presence of other traumatic injuries, were obtained. Fractures were classified according to location based on review of radiographs. Types of fixation were recorded: intramedullary nail, PF-LCP (Figure 1), cannulated screw, dynamic hip screw, and a combination of fixation types (Table 2). Follow-up information was collected with routine visit data—weight-bearing status and review of radiographs—up to 12 weeks postoperatively (Tables 3 and 4). We chose 12 weeks for the minimum follow-up period because union of these fractures in children typically can be expected by 12 weeks from the time of treatment and because our retrospective data were more complete at that time point than in subsequent time points due to many patients being lost to follow-up beyond that period. In cases of early implant mechanical failure, timing and mechanism of failure were recorded.
Table 1. Mechanism and Frequency of Injury by Fracture Classification
| Mechanism of Injury | Frequency | Subtrochanteric | Delbet I | Delbet II | Delbet III | Delbet IV |
|---|---|---|---|---|---|---|
| Fall from height | 14/64; 21.8% | 3 | 0 | 0 | 3 | 8 |
| Same level fall | 13/64; 20.3% | 6 | 1 | 3 | 0 | 3 |
| Pedestrian struck | 11/64; 17.2% | 5 | 0 | 4 (1) | 0 | 2 |
| Motor vehicle collision | 10/64; 15.6% | 3 | 0 | 6 (1) | 0 | 1 |
| Pathologic fracture | 6/64; 9.4% | 0 | 0 | 0 | 3 (2) | 3 |
| All-terrain vehicle accident | 5/64; 6.3% | 2 | 0 | 0 | 2 | 1 |
| Gunshot wound | 1/64; 1.6% | 1 | 0 | 0 | 0 | 0 |
| Repeated stress | 1/64; 1.6% | 0 | 0 | 0 | 1 | 0 |
| Direct blow | 1/64; 1.6% | 0 | 0 | 0 | 0 | 1 |
| Unknown cause | 2/64; 3.1% | 1 | 0 | 0 | 0 | 1 |
Figure 1. Proximal femoral fracture in a 3-year-old boy.

Table 2. Fracture Classification by Fixation Method
| Fracture Classification | PF-LCP | Intramedullary Nail | Compression Hip Screw | Cannulated Screws | Combination |
|---|---|---|---|---|---|
| Delbet I | 0 | 0 | 0 | 1 | 0 |
| Delbet II | 2 (2) | 0 | 6 | 4 | 1 |
| Delbet III | 5 (2) | 0 | 2 | 1 | 1 |
| Delbet IV | 8 | 0 | 12 | 0 | 0 |
| Subtrochanteric | 11 | 8 | 2 | 0 | 0 |
Failures indicated by ().
Table 3. Fracture Classification by Weight-Bearing Status and Spica Cast Application
| Fracture Classification | Non-Weight-Bearing | Touch Down Weight-Bearing | Weight-Bear as Tolerated | Spica Cast* |
|---|---|---|---|---|
| Subtrochanteric | 11 | 9 | 1 | 3 |
| Delbet I | 0 | 1 | 0 | 0 |
| Delbet II | 12 (2) | 1 | 0 | 0 |
| Delbet III | 6 (2) | 3 | 0 | 0 |
| Delbet IV | 7 | 12 | 1 | 1 |
Failures indicated by (). *Spica casting was not used as a single fixation method in any patient; the spica cast column denotes the number of patients in whom a spica cast was used in conjunction with other fixation method.
Table 4. Fixation Method by Weight-Bearing Status and Spica Cast Application
| Fixation Method | Non-Weight-Bearing | Touch Down Weight-Bearing | Weight Bear as Tolerated | Spica Cast |
|---|---|---|---|---|
| PF-LCP | 18 (4) | 8 | 0 | 3 |
| IM Nail | 3 | 4 | 1 | 0 |
| CHS | 9 | 12 | 1 | 1 |
| Cannulated Screws | 5 | 1 | 0 | 0 |
| Combination | 1 | 1 | 0 | 0 |
Failures indicated by (). *Spica casting was not used as a single fixation method in any patient; the spica cast column denotes the number of patients in whom a spica cast was used in conjunction with other fixation method.
For continuous variables, t-tests were applied. For categorical variables, chi-square or Fisher tests were used. Differences were considered statistically significant for p < 0.05.
Results
Sixty-one children with 64 proximal femoral fractures met inclusion criteria. The average age at presentation in the 48 males and 13 females was 10.4 years (range, 3 to 17 years). Twenty-six fractures were treated with PF-LCPs and 38 with fixation other than PF-LCP, including compression hip screw, intramedullary nail, cannulated screws, and a combination of methods. The average age of patients treated with PF-LCP was 7.7 years compared to 12.2 years in those treated with other methods (p<0.001). The most common mechanism of injury was a fall from a height (14/64, 21.8%); the rest of the mechanisms are summarized in Table 1.
Fixation failure was identified in four of 64 fractures (6.2%), all in patients with PF-LCP fixation (4 of 26, 17.4%); no failures were seen with other fixation constructs (p<0.05). One of the four fixation failures was identified at the 2-week postoperative visit and three at 6-week postoperative visits. Failure of screws (breakage and bending) occurred in three of the four failures (Figures 2 and 3), and loss of reduction occurred in one.
Figure 2. A) Bilateral proximal femoral fracture in a 4-year-old girl. B) Intraoperative fluoroscopic view. C) After fracture fixation. D) First radiograph with evidence of failure. E) After revision.
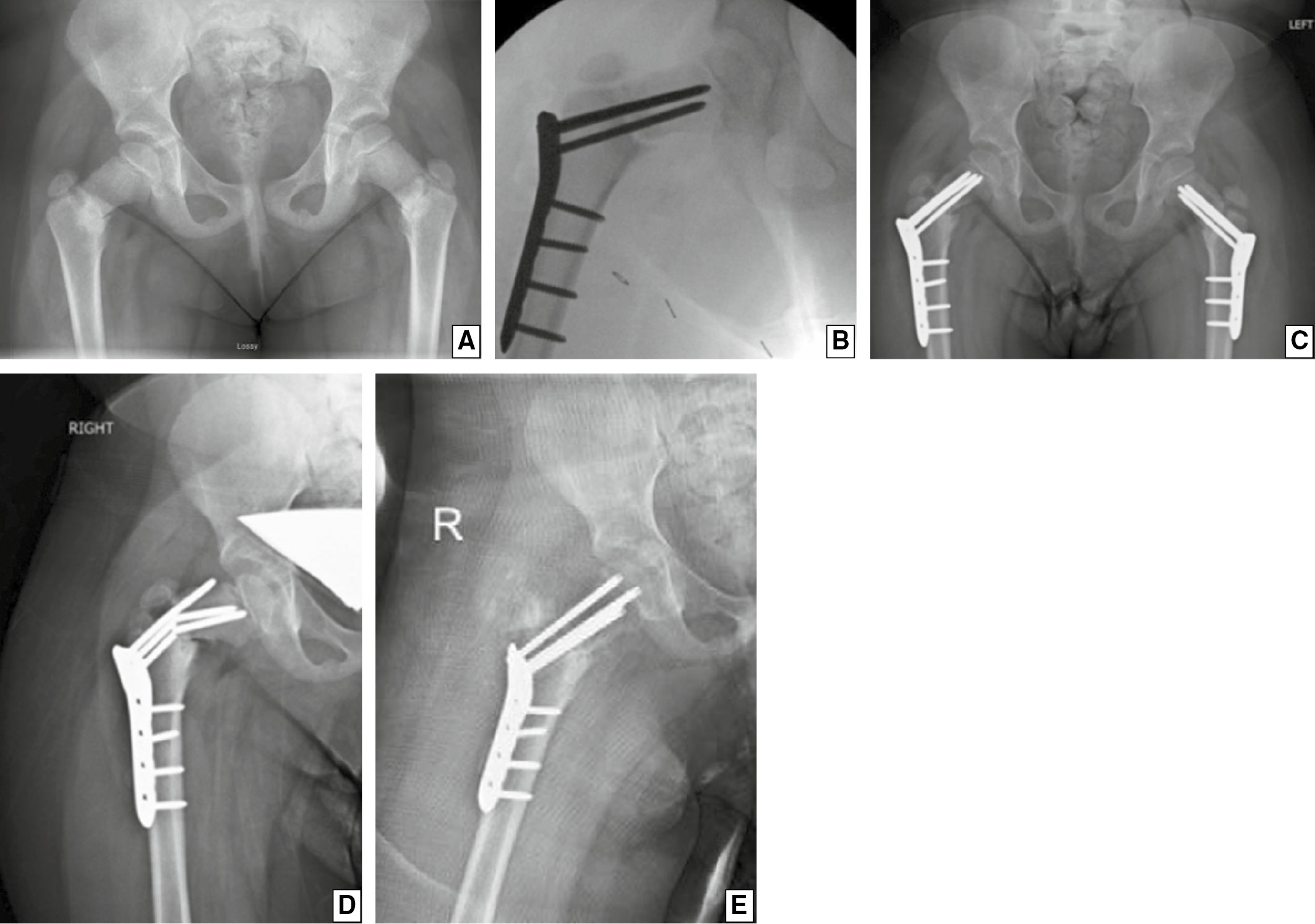
Figure 3. A) Proximal femoral fracture in a 6-year-old boy. B) Intraoperative fluoroscopic view. C) After fracture fixation. D) First radiograph with evidence of failure. E) After revision.

Discussion
A variety of methods are available for surgical stabilization of fractures of the proximal femur in the pediatric population. In this retrospective review of a series of these injures, failures were uncommon and occurred only in patients treated with proximal femoral locking compression plates.
Pediatric proximal femoral fractures are a relatively rare injury that may have serious and lasting complications.6,13,14 They usually are a result of high-energy trauma and frequently are not isolated injuries.15 A variety of fixation modalities are available for fixation of these fractures, and the decision for which modality to use is based on multiple factors.2,16,17 A relatively new implant is the PF-LCP, which was primarily designed to stabilize osteotomies following deformity correction surgeries in children and adults. Our study was designed to examine the use of PF-LCPs in only fractures, and it includes a larger population than has been studied previously. Based in part on higher reported failure rates with these implants in studies of adult proximal femoral fractures, we hypothesized that PF-LCPs would result in higher failure rates in pediatric proximal femoral fractures than other fracture fixation options.
Early biomechanical studies of the PF-LCP demonstrated high success rates in adults and showed the PF-LCP to be superior to conventional fixation in osteoporotic bone due to better mechanical fixation of the implant to the bone. Soon after introduction into clinical use, however, early studies showed inconsistent results with increased stiffness and a trend towards a higher number of load cycles before failure relative to other implants.18 Mixed results soon followed, with complication rates of 38% and 70% in two clinical studies.9,19 Those failures included loss of fixation, screw backout, screw fracture, and plate fracture.
Since its introduction, the PF-LCP has been used and studied for a variety of indications. Streubel et al.,9 in a series of 30 proximal femoral fractures with locking plate fixation in adults, showed a failure rate of 38%. Joeris et al.11 studied 30 pediatric patients with PF-LCP fixation for a variety of conditions, only three of which were fractures. None of these three patients had plate failures; however, 29 of 30 plates did require removal at a range of 6 to 34 months. We choose to focus our study on patients being treated for fractures without the inclusion of those with planned osteotomies.
We hypothesized that there would be an increased early mechanical failure rate in fractures treated with the PF-LCP compared to other fixation modalities. Of the 64 fractures in our study, there were four early failures, all of which occurred in patients treated with PF-LCPs, while no failures occurred with other stabilization options. The reason for these failures remains unclear. The rigidity of the PF-LCP does not allow for compression across the fracture site for femoral neck fractures, which could have contributed to mechanical failure in some of these cases.8,19 As this was a retrospective study with different implant types and different treating surgeons in patients of various ages, there was no single surgical technique or postoperative protocol for weight-bearing, and some patients carried comorbid conditions into their traumatic event; specifically, one of the patients with bilateral failure had a diagnosis of glioblastoma. There are many factors that could have led to the failures in our patient population, including the fracture location and pattern, comorbid conditions, treating surgeon, and postoperative protocol; nevertheless, the implant choice seemed to emerge as an important factor in the failures within this pediatric patient population particularly in the combination of PF-LCP plates and basicervical femoral neck fractures.
Islam et al.20 reported a series of 43 patients treated with PF-LCPs for both planned osteotomies and fractures; only three of the 43 patients had fractures. They showed good results with no hardware loosening among all patients, but their fracture sample size was small. All three fractures were classified as subtrochanteric fractures, and all healed successfully by 6 months with no complications apparent. The small sample size of these fractures makes it difficult to compare the results of these studies with our results.
There are limitations with this study. Because data were collected retrospectively, the choice of treatment modality was based on the information available at the time regarding patient age, fracture pattern, comorbid injuries, and surgeon preference. Additionally, patient demographics were fairly different, with a significantly different age of patients between the two groups. Another limitation of this study was the relatively short follow-up period. Union had been achieved in all patients in the non-PF-LCP group by the 12-week follow-up visit, so we believed that no additional implant failures would develop beyond that period. Also, many of our patients were lost to follow-up beyond 12 weeks, further limiting the amount of data available. There are a few strengths to this study as well. This is a sizeable patient population for a single institution and for a fairly rare fracture location in children. This study compares a number of different implant types and fracture locations.
In summary, there is a scarcity of literature concerning the use of PF-LCPs in pediatric proximal femoral fractures; this is likely due to the relatively recent introduction of the implant itself, the low incidence of these fractures, and the many implant choices available. Our results show that there is a higher rate of early mechanical failure with PF-LCPs, specifically in femoral neck fracture, than with other modalities. The increased risk of failure with PF-LCPs should be carefully considered before these implants are chosen.
Additional Links
- POSNA Annual Meeting Abstracts: Proximal Femoral Fracture
- POSNA Study Guide: Femur Fracture
Disclaimer
The authors report no conflicts of interest related to this manuscript.
References
- Wu C, Ning B, Xu P, et al. Efficacy and complications after delayed fixation of femoral neck fractures in children. J Orthop Surg. 2020;28(1):1-6.
- Boardman MJ, Herman MJ, Buck B, et al. Hip fractures in children. J Am Acad Orthop Surg. 2009;17(3):162-173.
- Patterson JT, Tangtiphaiboontana J, Pandya NK. Management of pediatric femoral neck fracture. J Am Acad Orthop Surg. 2018;26(12):411-419.
- Davison BL, Weinstein SL. Hip fractures in children: a long-term follow-up study. J Pediatr Orthop. 1992;12(3):355-358.
- Chung M, Kwon S-S, Cho B, et al. Incidence and risk factors of hardware-related complications after proximal femoral osteotomy in children and adolescents. J Pediatr Orthop B. 2018;27(3):264-270.
- Sankar WN, Mehlman CT. The community orthopaedic surgeon taking trauma call: pediatric femoral neck fracture pearls and pitfalls. J Orthop Trauma. 2019;33:S22.
- Singh KA, Chandankere V, Shah H. Does the timing of treatment affect complications of pediatric femoral neck fractures? J Orthop. 2020;22:207-212.
- Viberg B, Rasmussen KMV, Overgaard S, Rogmark C. Poor relation between biomechanical and clinical studies for the proximal femoral locking compression plate: a systematic review. Acta Orthop. 2017;88(4):427-433.
- Streubel PN, Moustoukas MJ, Obremskey WT. Mechanical failure after locking plate fixation of unstable intertrochanteric femur fractures. J Orthop Trauma. 2013;27(1):22-28.
- Dial BL, Lark RK. Pediatric proximal femur fractures. J Orthop. 2018;15(2):529-535.
- Sanders S. Egol KA. Adult periarticular locking plates for the treatment of pediatric and adolescent subtrochanteric hip fractures. Bull NYU Hosp Jt Dis. 2009;67(4):370-373.
- Joeris A, Aduigé L, Ziebarth K, et al. The locking compression paediatric hip plate™: technical guide and critical analysis. Int Orthop. 2012;36(11):2299-2306.
- Spence D, DiMauro J-P, Miller PE, et al. Osteonecrosis after femoral neck fractures in children and adolescents: analysis of risk factors. J Pediatr Orthop. 2016;36(2):111-116.
- Papalia R, Torre G, Maffulli N, et al. Hip fractures in children and adolescents. Br Med Bull. 2019;129(1):117-128.
- Caldwell L, Chan CM, Sanders JO, et al. Detection of femoral neck fractures in pediatric patients with femoral shaft fractures. J Pediatr Orthop. 2017;37(3):e164.
- Pavone V, Testa G, Riccioli M, et al. Surgical treatment with cannulated screws for pediatric femoral neck fractures: a case series. Injury. 2019;50(1):S40-S44.
- Pandey RA, John B. Current controversies in management of fracture neck femur in children: a review. J Clin Orthop Trauma. 2020;11(Suppl 5):S799-S806.
- Crist BD, Khalafi A, Hazelwood SJ, et al. A biomechanical comparison of locked plate fixation with percutaneous insertion capability versus the angled blade plate in a subtrochanteric fracture gap model. J Orthop Trauma. 2009;23(9):622-627.
- Glassner P, Tejwani N. Failure of proximal femoral locking compression plate: a case series. J Orthop Trauma. 2011;25(2):76-83.
- Islam SU, Henry A, Khan T, et al. The outcome of paediatric LCP hip plate use in children with and without neuromuscular disease. Musculoskelet Surg. 2014; 98(3):233-239.
