Current Concept Review
Management of Pediatric Proximal Humerus Fractures
1Department of Orthopaedic Surgery, University of California San Francisco, San Francisco, CA; 2University of California San Francisco School of Medicine, San Francisco, CA
Correspondence: Ishaan Swarup, MD, University of California, San Francisco, 747 52nd Street, OPC First Floor, Oakland, CA 94609. E-mail: [email protected]
Received: September 13, 2022; Accepted: November 21, 2022; Published: February 1, 2023
Volume 5, Number 1, February 2023
Abstract
Proximal humerus fractures have an outstanding potential to remodel due to their proximity to the proximal humeral physis. Fractures in young children can be treated nonoperatively with excellent outcomes. The incidence peaks in adolescent patients and these injuries most commonly occur after a fall or direct trauma. The muscle attachments of the proximal humerus act as deforming forces and anatomic structures such as the periosteum and biceps tendon may act as blocks to reduction. Operative management is uniformly indicated for patients with open fractures, ipsilateral elbow or forearm injury, associated neurovascular injury, or poly-trauma patients. Operative treatment may be further considered in older children with minimal growth remaining and with fractures that are considered significantly displaced by available classification systems. Unfortunately, there are significant challenges in recommending treatment based on displacement and age alone. The purpose of this paper is to review what is known about these injuries and how they can be treated in light of current deficiencies in the literature; this may stimulate further work to refine indications for treatment based upon age and displacement.
Key Concepts
- The proximal humerus physis is responsible for 80% of the growth of the entire bone, and proximal humerus fractures have tremendous potential to remodel.
- Proximal humerus fractures occur most commonly due to a fall or direct trauma but other causes include overuse injury and pathologic lesions.
- Treatment indications for pediatric proximal fractures are guided by age of the patient, fracture displacement, and associated injuries; the majority of these injuries may be treated nonoperatively.
- Outcomes after operative and nonoperative management of proximal humerus fractures are generally good.
Introduction
Proximal humerus fractures account for approximately 2% of all pediatric fractures and can be seen throughout childhood to adolescence.1 There have been several recent studies assessing indications for management, variability in practice, and outcomes after this injury. The purpose of this review is to describe the epidemiology, relevant anatomy, natural history, and recent literature on the indications and outcomes of pediatric proximal humerus fractures. We further highlight some of the difficulties in recommending treatment based upon age and displacement.
Epidemiology and Mechanism of Injury
The incidence of proximal humerus fractures is approximately 31.4 per 100,000 children.2 and peaks between 10–14 years of age.3 Studies have shown proximal humerus fractures to be up 3–4 times more common in males compared with females, though these numbers vary across studies.2,4–6 Proximal humerus fractures in children below the age of 2 years may occur during the birthing process or as a result of child abuse.7–10
Proximal humerus fractures most commonly result from a backwards fall onto an outstretched hand with an extended, abducted, and externally rotated arm. Direct trauma to the shoulder is another common cause of proximal humerus fractures with approximately one-third of all these fractures in children resulting from motor vehicle accidents. Sports-related injuries make up another quarter of all proximal humerus fractures.11
Pathologic fractures are another important cause of proximal humerus fractures in young patients and include unicameral bone cysts, aneurysmal bone cysts, nonossifying fibroma, and osteosarcoma.12 As these lesions expand, they weaken the bone and lead to pathologic fractures. Although rare, there are case reports of osteomyelitis of the humerus resulting in separation and displacement of the humeral physis.13 Finally, children participating in sports may be prone to overuse injuries such as “Little Leaguer’s shoulder” and avulsion fractures.4,14,15 Little Leaguer’s shoulder results in epiphysiolysis of the proximal humerus and occurs most commonly in baseball players between 11 and 16 years of age.16
Shoulder Development and Pertinent Anatomy
An appreciation of the anatomy of the proximal humerus is important for understanding the common fracture displacement patterns that are found. The main anatomic segments corresponding with the ossification centers of the proximal humerus include the shaft, the greater tuberosity, the lesser tuberosity, and the humeral head.17 The development of the proximal humerus begins at infancy with the development of pre-ossification centers that then begin to be replaced by osteoid in the first few months of life. These secondary ossification centers appear in the proximal humeral epiphysis at around 2-4 months, with the greater tuberosity ossification center appearing at 7-10 months.18–20 These ossification centers fuse by the age of 3 and continue to expand. Ossification of the humeral head is typically complete by the age of 13, with the lesser tuberosity being the last to ossify.20 There is debate whether there is a third ossification center developing by the age of 5 in the lesser tuberosity that joins the other centers at ages 6-7 or if the proximal humerus ossification center expands into the lesser tuberosity.19–21
The proximal humerus is the point of insertion for the supraspinatus, infraspinatus, and teres minor into the greater tuberosity, and the subscapularis inserts into the lesser tuberosity. The greater and lesser tuberosities are separated by the bicipital groove which runs the long head of the biceps tendon. Lateral to the bicipital groove is the insertion point for the pectoralis major, and medial to it the insertion of latissimus dorsi and teres major. The deltoid inserts into the shaft of the humerus laterally at the deltoid tuberosity.
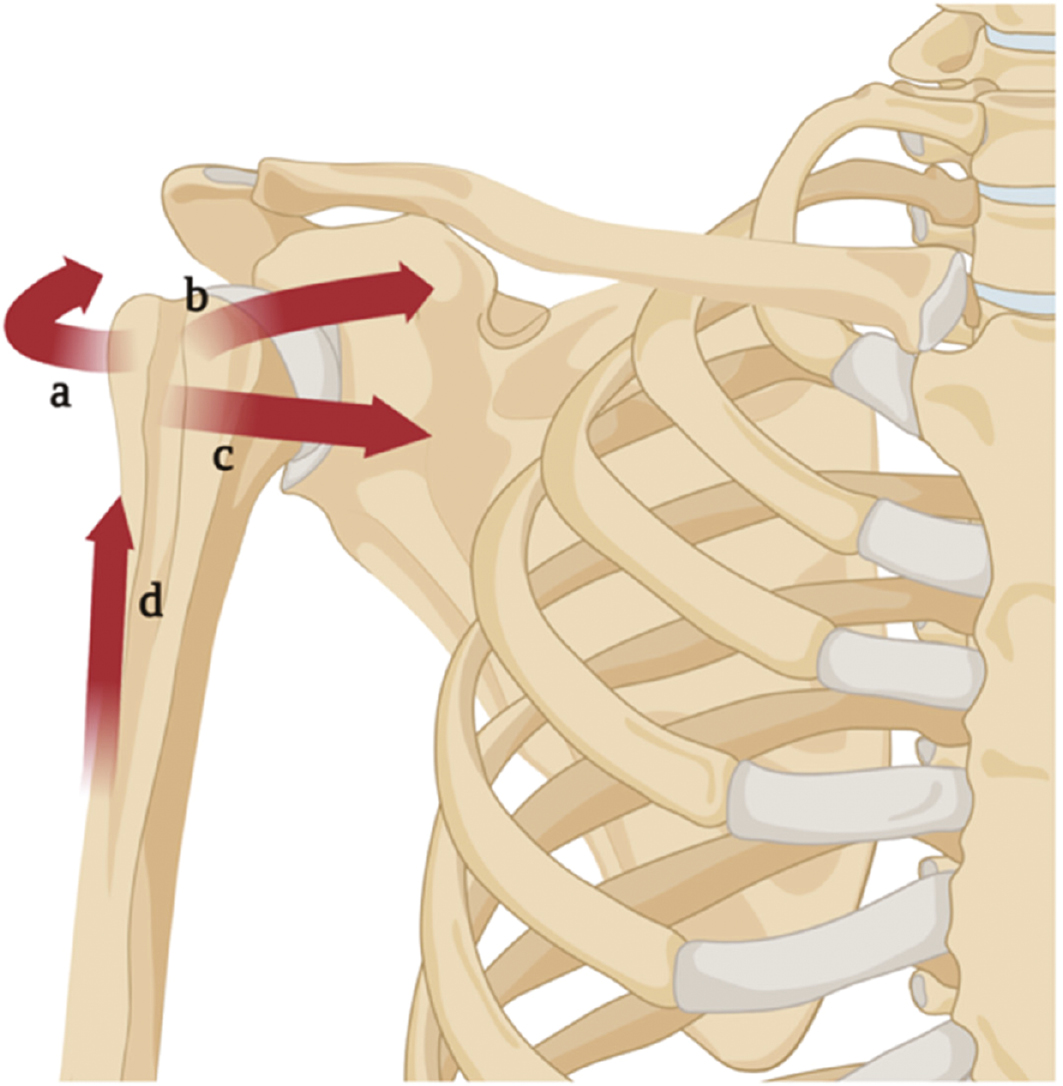
The many sites of muscle attachment act as deforming forces on the proximal humerus (Figure 1). The pectoralis major is the major deforming force of the proximal humerus and displaces the shaft medially and anteriorly. The greater tuberosity is externally rotated due to the forces exerted by the supraspinatus, infraspinatus, and teres minor while the lesser tuberosity is displaced anteromedially by the subscapularis.
Figure 1. Deforming forces around the proximal humerus. a) The supraspinatus, infraspinatus, and teres minor insert into and externally rotate the greater tuberosity. b) The subscapularis inserts into the lesser tuberosity and pulls the tuberosity anteromedially. c) The pectoralis major inserts into the intertubercular sulcus and displaces the shaft of the humerus anteromedially. d) The deltoid inserts into the deltoid tuberosity of the humeral shaft and abducts the humerus. Created with BioRender.com.
The neurovascular structures are intimately associated with the proximal humerus with the axillary artery and brachial plexus in proximity. Notably, the major blood supply to the humeral head is via the posterior circumflex humeral artery and significant displacement can lead to avascular necrosis of the humeral head.22 The axillary nerve runs inferior to the glenoid and into the deltoid which can be injured during the initial fracture or iatrogenically during surgical fixation. Additionally, the long biceps tendon runs intraarticularly in the glenohumeral joint. Its proximity to the humeral head can complicate closed reduction if becomes entrapped from the fracture or during closed reduction of proximal humerus fractures.23 Other structures of the shoulder which may block reduction of proximal humerus fractures include periosteum, deltoid muscle, joint capsule, and bony comminution.24–26
Development and Natural History
A common feature of proximal humerus fractures is the ability to remodel, primarily due to the thick periosteum and its anatomic location relative to the physis. The proximal humerus physis is responsible for 80% of the growth of the entire bone, giving the proximal humerus extraordinary remodeling potential in children. This allows even severely displaced fractures to be treated nonoperatively, and significant displacement or angulation tends to remodel in younger children without any long-term sequelae in function or cosmesis (Figure 2).27
Figure 2. This two-year-old suffered a right upper extremity injury as a result of nonaccidental trauma. At 2 weeks, she was referred to an orthopaedic practice for management and a nonoperative approach was chosen. Eighteen months later, her fracture remodeled and her function was normal. Case courtesy of Ken Noonan, MD.

While surgical neck fractures at the meta-diaphyseal junction can occasionally occur (Figure 3), most proximal humerus fractures in children are metaphyseal with variable involvement of the growth plate. Physeal fractures are seen in adolescents due to the rapid growth at this age leading to a weakened physis.27,28 With physeal fractures, growth arrest may occur leading to functional and cosmetic issues.
Figure 3. This is a 6-year-old girl who sustained a proximal humerus fracture. Despite the displacement, she was treated nonoperatively. At 4.5 months, she had excellent healing and remodeling of the fracture displacement with no pain or residual dysfunction. If the fracture occurred in adolescence, the subsequent length discrepancy is not associated with functional outcomes and is not often apparent.27

The majority of proximal humerus fractures in pediatric patients do well with nonoperative management. In neonates, complete remodeling of proximal humeral fractures is observed within 6 months, with clinical union seen as early as 2 weeks.29 A systematic review looking of functional outcomes in pediatric patients with proximal humeral fractures treated nonoperatively showed that Constant Scores were at 100 for patients aged 0-16 who, on average, had 3 years follow-up.30 Only 4% of patients had limb shortening, 7% endorsed pain, and 6% had restrictions in range of motion.30 From this, it would appear that the natural history of nonoperatively treated proximal humerus fractures results in good outcomes in young patients with remodeling potential. Unfortunately, it is difficult to conclude the same in published series of older patients treated nonoperatively, as some patients in these institutions would have been selected for operative fixation.
Classification Systems
The Salter Harris system can be used to describe proximal humerus physeal fractures. Type I Salter Harris fractures disrupt the physis only while type II fractures involve a break through the physis and extension into the metaphysis. Type III fractures extend intraarticularly and type IV fractures involve the epiphysis, physis, and metaphysis. Pediatric proximal humerus fractures are most often graded by the Neer-Horowitz system.31 Grade I fractures are less than 5 mm displaced, grade II fractures are displaced no more than 1/3 the shaft width, grade III fractures are displaced between 1/3 and 2/3 the shaft width, and grade IV fractures are displaced more than 2/3 the shaft width (Table 1). Neer-Horowitz grade III and IV fractures have been associated with worse functional outcomes.4 Lastly, fracture-dislocations of the proximal humerus can occur in older children but are rare.
Table 1. Neer-Horowitz Classification of Proximal Humerus Fractures
| Grade | Displacement |
|---|---|
| I | <5 mm |
| II | <1/3 of shaft width |
| III | 1/3 - 2/3 of shaft width |
| IV | >2/3 of shaft width |
In order for fracture classification systems to be valuable, they must allow providers to fully describe the fracture pattern with high reliability, and the different grades would correlate with the natural history of nonoperative management and thus suggest which grades may benefit from operative management. Orthogonal imaging is usually indicated in pediatric patients similar to adult patients, but proximal humerus fractures are three-dimensional injuries that are difficult to fully characterize on radiographs that may be taken at different angles to the shoulder. Most trauma series are taken supine, and thus, are likely to be different to those taken upright. Finally, while the Neer-Horowitz system uses displacement to characterize the fracture, angulation as described by Burke et al. is also an important consideration for treatment.32
Treatment
Indications
Treatment indications for pediatric proximal fractures are guided by age of the patient, fracture displacement, and associated injuries. Due to the immense remodeling potential of the physis, operative treatment in young children is rarely necessary.30 Although the exact age cut off varies in the literature, generally until the age of 10, nonoperative management yields excellent outcomes even with severe displacement.31,33 Older patients are unable to accommodate for significant displacement and can have decreased range of motion from persistent malalignment.24,34,35 While there have been numerous guidelines based on translation (Neer-Horowitz classification) or angulation, there is not yet a clear consensus on indications for operative management (Table 2).
Table 2. Indications for Operative Management of Proximal Humerus Fractures as Reported in the Literature
| Indication for Operative Management | |
|---|---|
| Burgos-Flores et al. 1993 | 30% angulation or >50% displaced in patients >13 years |
| Beaty et al. 1992 | 100% translation or >70 degree angulation, <5 years; >50% translation or angulation <70 in younger and >40 in older children, age 5-10 years Translation >50% or angulation >40% in patients >11 years |
| Dobbs et al. 2003 | >75 degree angulation in patients 7 years and under; >60 degree angulation in patients 8 to 11 years >45 degree angulation in patients >11 years |
| Pahlavan et al. 2011 | Nonoperative, <10 years; Case-by-case basis in patients 10-13 years Displaced fracture in patients >13 years |
| Hutchinson et al. 2011 | Neer-Horowitz Grade IV or >40 degree angulation in patients >12 years |
| Lefèvre et al. 2014 | >100% translation and/or angulation >70 degrees, patients <10 years; >50% translation and/or angulation >40 degrees, patients 10-13 years; >30% translation and/or angulation >20 degrees, patients >13 years |
| Popkin et al. 2015 | Neer-Horowitz Grade III and IV fractures in patients > 11 years |
| Binder et al. 2016 | >60 degree angulation in patients < 12 years; >30 degree angulation in patients > 11 years |
| Cruz et al. 2018 | Neer-Horowitz Grade III and IV >60 degree angulation in patients <10 years; >30 degree angulation in patients >9 years |
| Thomson et al. 2021 | Adolescent patients with Neer III and IV |
In some cases, recommendations are clear. For example, patients with associated injuries such as open fractures, vascular injury, and polytrauma are usually managed surgically given the concomitant injury and in order to minimize risk of complications (Figure 4).36 In contrast, for obstetric fractures, the treatment is uniformly swaddling with excellent outcomes.7,29 The guiding principle is nonoperative management in younger children and a lower threshold to operate in adolescents with impending closing physes. Overall, there has been a decreasing rate of operative management of adolescent proximal humerus fractures in recent years with considerable geographic variation.6 There is also difference in management depending on the treating hospital with higher rate of operative management in general hospitals compared to children’s hospitals which demonstrates this lack of consensus.5,6
Figure 4. This is a 14-year-old patient who was injured when his ATV ran into a barn. Operative fixation of all three fractures was performed. Case courtesy of Ken Noonan, MD.

Management of Fractures with Acceptable Alignment
Nonoperative management consists of simple immobilization with a sling or a hanging arm cast. A shoulder spica cast is poorly tolerated in older children and rarely needed in younger children, so it is not commonly used by the authors. When there is minimal displacement, a simple sling and swathe or shoulder immobilizer can be used to position the humerus against the torso. The sling can be removed for hygiene and dressing, with parental supervision in younger children. A hanging arm cast can be helpful to apply gravity traction to the fracture site and to slow down more active patients. To be fully effective, the patient needs to sleep upright for the first 10 to 14 days and until the fracture becomes sticky. For nonoperative management, immobilization of 2-3 weeks in neonates and 3-4 weeks in children is sufficient as guided by pain and radiographic healing at follow-up.11
Closed Reduction of Proximal Humerus Fractures
Two of the most difficult questions in managing proximal humerus fractures are 1) when does a fracture need to be reduced and 2) where and how should it be reduced?
Significantly displaced fractures such as Neer-Horowitz grade III and IV fractures have higher odds of shortening and limited motion, with limitations in abduction being the most common.37 The most important factors that affect that decision are the age of the patient and the degree of displacement, yet different results can occur for relatively similar patients treated similarly (Figure 5).
Figure 5. Two adolescent males with proximal humerus fractures treated with closed reduction and sling immobilization in the emergency room with different outcomes likely as a result of patient age at injury. Case courtesy of Ken Noonan, MD.

The authors recognize that the majority of available literature cannot make recommendations on when to attempt a reduction as most recommendations (Table 2) are based on Level 4-5 evidence. As such, our recommendations should be considered as a continuation of this problem. Despite this limitation, we currently consider reduction for fractures displaced greater than 33% (Neer III or IV) or fractures with greater than 40 degrees of angulation in patients within 2 years of skeletal maturity (boys ≥ 14 years, girls ≥ 12 years).
Once a patient is indicated for reduction, the team will need to consider if the fracture should be reduced in the emergency room (ER) or in operating room (OR). On one hand, if the fracture can be reduced easily in the ER, that saves time and resources, yet these can be challenging to reduce unless the patient is deeply sedated with several staff needed to stabilize the patient while traction and manipulation is applied. The authors advocate that an attempt in the ED seems reasonable if adequate resources and safe deep sedation can be obtained. On the other hand, if the fracture is significantly displaced with obvious soft tissue interposition (Figure 6) then an operative reduction with the option to use internal fixation may be prudent.
Figure 6. This 12-year-old girl has soft tissue interposition that may be best managed by reduction. Case courtesy of Ken Noonan, MD.

Fractures that do not immediately need surgery (open fracture, neurovascular injury, etc.) can be treated with semi-elective reduction; in fact, there may be some advantage to waiting a few days. The radiographic images in the ED are almost always supine (and look worse) and are not upright. In addition, the effect of gravity and time may provide surprising results (Figure 7).
Figure 7. This 14-year-old female was managed with a hanging arm cast and had reduction of the deformity by 1 week. Surgery was avoided. Case courtesy of Steve Frick, MD.

Open Reduction of Proximal Humerus Fractures
Approximately 10-30% of fractures with persistent displacement will require an open reduction due to entrapment of soft tissue structures, most commonly the biceps tendon.23,37 When closed reduction does not allow for acceptable reduction, the fracture can be opened to remove the entrapped tissue that blocks reduction. Subtle residual displacement in younger children after closed reduction can be tolerated. When open reduction is needed, the authors utilize a deltopectoral approach with careful avoidance of the axillary artery/nerve during exposure or fixation. While the deltopectoral approach is the most commonly used, it provides limited exposure of the posterolateral proximal humerus. The anterolateral approach utilizes a deltoid splitting interval but is limited distally due to the anterior branch of the axillary nerve that crosses 4 to 6 cm distal to the acromion.38 Surgeons should be aware of the challenges of each approach and understand the fracture in three-dimensional space prior to choosing the approach.
Skeletal Stabilization Techniques
Fixation techniques include pins, screws, plates, elastic nails, or external fixators, all of which have demonstrated excellent results under the right conditions (Table 3).4,37 The most commonly used techniques are percutaneous pins or screws and elastic nailing, with comparable results.39 Percutaneous pin/screws or retrograde elastic nailing is minimally invasive compared to a plate and screw construct, which is usually unnecessary in children. Freislederer et al. describe irreducible fractures in adolescent patients that were treated with open reduction and plate and screw fixation.40 Advantages include avoiding direct injury to the physis with the downside being another open surgery in 3-6 months for plate removal. With elastic nails, there is excellent fracture stability even in severely displaced fractures with good clinical outcomes but has a longer operative time, increased blood loss, and learning curve compared to percutaneous pinning.11,41–43
Table 3. Comparison of Different Methods to Stabilize Proximal Humerus Fractures
| Technique | Advantages | Disadvantages |
|---|---|---|
| Pinning |
|
|
| Plate/screws |
|
|
| Elastic nail |
|
|
| External fixator |
|
|
Excellent postoperative outcomes have been reported with pin fixation.44,45 Hutchinson et al. compared pinning to flexible nailing and found longer operating time for nailing (121 min vs. 63 min) with higher blood loss but a higher complication rate in the pinning group (41% vs. 4%).43 Complications in the pinning group were pin site infections and pin migration, but similar rates have not been noted in other studies. Both strategies rendered excellent fracture stability and improvement in fracture displacement. Kraus et al. compared pinning to nailing and found no functional or radiographic outcome difference, yet percutaneous pinning led to a shorter hospital stay and shorter time to implant removal.44
There have also been advancements using only one elastic nail with shortened surgical time to 49 minutes with maintenance of reduction.39,46 An advantage to percutaneous pinning is if the pins are left outside of the skin, a second anesthetic can be avoided, but at the greater risk of pin site immigration or infections. Thankfully these fractures become stable within three weeks and thus pins can be pulled before significant deep infections could develop. One meta-analysis demonstrated slightly better functional outcomes in ESIN (98%), followed by pinning (95%), and nonoperative management (91%) with similar rates of complications (9% in nailing vs 7% in pinning).47 The use of external fixators is reserved for rare cases of glenohumeral dislocation, which occurs in 2% of pediatric proximal humerus fractures.48
Patient Outcomes
Nonoperative treatment when properly pursued rarely results in any long lasting complications. Nonunions have not been reported in the literature, and generally malunions are well tolerated in the shoulder due to the large arc of motion.11,37 Exceptions are for older children as limitations in range of motion or functional limitations can be seen in patients older than 13 who were treated nonoperatively.24,49 Baker et al. reviewed 69 pediatric patients with nondisplaced or minimally displaced proximal humerus fractures.28 Early complications were seen in 13% of patients, of which were reduced range of motion (7.2%), pain (4.3%), and decreased strength (1.4%). There were no cases of premature physeal closure, and all patients were managed with physical therapy or observation with none requiring operative intervention. Bahrs et al. showed superior Constant scores with nonoperatively treated patients although there were only 10 nonoperatively-treated patients in this series.23 Pahlavan et al. showed in their systematic review, 6% of nonoperatively treated patients had limited range of motion, 7% had pain, and 4% had shortening.37 Health-related quality of life has been shown to be excellent following nonoperative management of proximal humerus fractures.50 It is exceedingly rare for a proximal humerus fracture managed nonoperatively to be converted to operative intervention, and there are arguments made to minimize routine monitoring radiographs or to follow up with allied health providers.28,51
Operative management can also lead to complications of pain, weakness, and loss of motion and include infection and neurovascular injury. Pin site infection can be a common complication of percutaneous pinning but rarely leads to osteomyelitis of the humeral head.52,53 In children, avascular necrosis of the humeral head is a rare complication due to the rich periosteum and blood supply compared to adults. Hutchinson et al. demonstrated higher complication rates in the percutaneous pinning group up to 41% due to pin tract infections and pin migration.43 However, pin site infections generally resolve after pin removal, and clamping the pins has been utilized to minimize the risk of migration.54 The use of smooth pins has been associated with pin migration, but terminally threaded pins decrease this risk and this technique is our preferred choice of fixation for these fractures.54 With percutaneous pinning, there is also risk of iatrogenic injury to the axillary nerve or artery, but this is exceedingly rare.43,55 Elastic nails have also been associated with nail penetration into the joint space, and careful fluoroscopic and range of motion examination must be performed prior to leaving the operating room.56 For elastic nails, skin infection at the nail insertion site and temporary injury to the radial nerve have been reported.43,57 Growth plate injury can be seen in both operative and nonoperative management, and anatomic reduction in older children and minimizing number of passes of the nail or pin through the growth plate can minimize injury.10
Summary
Proximal humerus fractures in pediatric patients often occur after a fall and the incidence peaks in young adolescents. It is important to understand the anatomy of the proximal humerus in determining fracture displacement and fixation. Specifically, the muscles of the proximal humerus function as deforming forces and in some cases, may also block fracture reduction. Neurovascular structures are important to recognize at initial assessment and intraoperatively to avoid iatrogenic injury during fixation. The proximal humerus physis has outstanding remodeling potential, and the majority of fractures in young children can be treated nonoperatively. Long-term studies have shown excellent functional outcomes in young children treated nonoperatively. However, operative management may be considered in older children with decreased remodeling potential and displaced fractures. There are several techniques for operative management, but percutaneous fixation and elastic nailing are most commonly used in pediatric patients. Overall, patients have good outcomes with operative and nonoperative management of proximal humerus fractures. Additional studies are needed to compare surgical techniques and guidelines are needed to reduce practice variation.
Additional Links
- JBJS Essential Surgical Techniques: Percutaneous Pinning of Pediatric Proximal Humeral Fractures
- POSNA Study Guide—Proximal Humerus Fractures
Disclaimer
No funding was received. The authors have no conflicts of interest to report.
References
- Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop Part B. 1997;6:79-83.
- Hannonen J, Hyvönen H, Korhonen L, et al. The incidence and treatment trends of pediatric proximal humerus fractures. BMC Musculoskelet Disord. 2019;20:571.
- Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64:407–414.
- Popkin C, Levine W, Ahmad C. Evaluation and management of pediatric proximal humerus fractures. J Am Acad Orthop Surg. 2015;23:77-86.
- Cruz Jr AI, Kleiner JE, Gil JA, et al. Inpatient surgical treatment of paediatric proximal humerus fractures between 2000 and 2012. J Child Orthop. 2018;12:111-116.
- Kim AE, Swarup I. Decreasing rate of operative management of proximal humerus fractures in adolescents: a national database study: original research. JPOSNA®. 2022;4. https://doi.org/10.55275/JPOSNA-2022-0047.
- Basha A, Amarin Z, Abu-Hassan F. Birth-associated long-bone fractures. Int J Gynecol Obstet. 2013;123:127-130.
- Dias E. Bilateral humerus fracture following birth trauma. J Clin Neonatol. 2012;1:44-45.
- Kaya B, Daglar K, Kirbas A, et al. Humerus diaphysis fracture in a newborn during vaginal breech delivery. Case Rep Obstet Gynecol. 2015;2015:489108.
- Binder H, Schurz M, Aldrian S, et al. Physeal injuries of the proximal humerus: long-term results in seventy two patients. Int Orthop. 2011;35:1497-1502.
- Lefèvre Y, Journeau P, Angelliaume A, et al. Proximal humerus fractures in children and adolescents. Orthop Traumatol Surg Res. 2014;100:S149-S156.
- Ortiz EJ, Isler MH, Navia JE, et al. Pathologic fractures in children. Clin Orthop Relat Res. 2005;432:116-126.
- Wyers MR, Samet JD, Mithal LB. Physeal separation in pediatric osteomyelitis. Pediatr Radiol. 2019;49:1229-1233.
- Carson WG, Gasser SI. Little leaguer’s shoulder. Am J Sports Med. 1998;26:575-580.
- Neogi DS, Bejjanki N, Ahrens PM. The consequences of delayed presentation of lesser tuberosity avulsion fractures in adolescents after repetitive injury. J Shoulder Elbow Surg. 2013;22:e1-e5.
- Osbahr DC, Kim HJ, Dugas JR. Little league shoulder. Curr Opin Pediatr. 2010;22:35-40.
- Pinkas D, Wiater JM. Chapter 37 - Functional anatomy of the shoulder? In: Placzek JD, Boyce DA, eds. Orthopaedic Physical Therapy Secrets, Third Edition. St Louis, MO: Elsevier; 2017:318-326.
- Carson S, Woolridge DP, Colletti J, et al. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53:41-67, v.
- Shrader MW. Proximal humerus and humeral shaft fractures in children. Hand Clin. 2007;23:431-435, vi.
- Bachman D, Santora S. Orthopedic trauma. In: Textbook of Pediatric Emergency Medicine. Philadephia, PA: sLippincott Williams & Wilkins; 2006:1537.
- Benjamin HJ, Hang BT. Common acute upper extremity injuries in sports. Clin Pediatr Emerg Med. 2007;8:15-30.
- Hettrich CM, Boraiah S, Dyke JP, et al. Quantitative assessment of the vascularity of the proximal part of the humerus. J Bone Joint Surg Am. 2010;92:943-948.
- Bahrs C, Zipplies S, Ochs BG, et al. Proximal humeral fractures in children and adolescents. J Pediatr Orthop. 2009;29:238-242.
- Dameron TBJ, Reibel DB. Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am. 1969;51:289-297.
- Pandya NK, Baldwin KD, Wolfgruber H, et al. Humerus fractures in the pediatric population: an algorithm to identify abuse. J Pediatr Orthop B. 2010;19:535-541.
- King ECB, Ihnow SB. Which proximal humerus fractures should be pinned? treatment in skeletally immature patients. J Pediatr Orthop. 2016;36:S44-S44.
- Della-Giustina K, Della-Giustina DA. Emergency department evaluation and treatment of pediatric orthopedic injuries. Emerg Med Clin North Am. 1999;17:895-922.
- Baker C, Larson N, Shaughnessy W, et al. Rate of complications and subsequent shoulder complaints for non-operatively managed pediatric proximal humerus fractures. Front Surg. 2020;7:48.
- Sherr-Lurie N, Bialik GM, Ganel A, et al. Fractures of the humerus in the neonatal period. Isr Med Assoc J. 2011;13:363-365.
- Binder H, Tiefenboeck TM, Payr S, et al. Treatment of proximal humerus fractures in children and young adolescents. Wien Klin Wochenschr. 2016;128:120-124.
- Neer CS, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop. 1965;41:24-31.
- Burke MC, Minnock C, Robbins CB, et al. Intraobserver and interobserver reliability of radiographic analysis of proximal humerus fractures in adolescents. J Pediatr Orthop. 2019;39:e125-e129.
- Larsen CF, Kiaer T, Lindequist S. Fractures of the proximal humerus in children. Nine-year follow-up of 64 unoperated on cases. Acta Orthop Scand. 1990;61:255-257.
- Beringer DC, Weiner DS, Noble JS, et al. Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop. 1998;18:31-37.
- Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA, et al. Fractures of the proximal humeral epiphysis. Int Orthop. 1993;17:16-19.
- Dobbs M, Luhmann S, Gordon J, et al. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003;23:208-215.
- Pahlavan S, Baldwin KD, Pandya NK, et al. Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop. 2011;5:187-194.
- Robinson CM, Murray IR. The extended deltoid-splitting approach to the proximal humerus. J Bone Joint Surg Br. 2011;93-B:387-392.
- Samara E, Tschopp B, Kwiatkowski B, et al. A single retrograde intramedullary nail technique for treatment of displaced proximal humeral fractures in children. JBJS Open Access. 2021;6:e20.00119.
- Freislederer F, Bensler S, Specht T, et al. Plate fixation for irreducible proximal humeral fractures in children and adolescents—a single-center case series of six patients. Children. 2021;8:635.
- Fernandez FF, Eberhardt O, Langendörfer M, et al. Treatment of severely displaced proximal humeral fractures in children with retrograde elastic stable intramedullary nailing. Injury. 2008;39:1453-1459.
- Rajan RA, Hawkins KJ, Metcalfe J, et al. Elastic stable intramedullary nailing for displaced proximal humeral fractures in older children. J Child Orthop. 2008;2:15-19.
- Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J Pediatr Orthop. 2011;31:617-622.
- Kraus T, Hoermann S, Ploder G, et al. Elastic stable intramedullary nailing versus Kirschner wire pinning: outcome of severely displaced proximal humeral fractures in juvenile patients. J Shoulder Elbow Surg. 2014;23:1462-1467.
- Schwendenwein E, Hajdu S, Gaebler C, et al. Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg. 2004;14:51-55.
- Chee Y, Agorastides I, Garg N, et al. Treatment of severely displaced proximal humeral fractures in children with elastic stable intramedullary nailing. J Pediatr Orthop Part B. 2006;15:45-50.
- Hohloch L, Eberbach H, Wagner FC, et al. Age- and severity-adjusted treatment of proximal humerus fractures in children and adolescents—A systematical review and meta-analysis. PLoS One. 2017;12:e0183157.
- Hong P, Rai S, Liu R, et al. Glenohumeral joint dislocation is rare in children with proximal humeral fractures: a descriptive study and literature review. BMC Musculoskelet Disord. 2022;23:36.
- Chaus GW, Carry PM, Pishkenari AK, et al. Operative versus nonoperative treatment of displaced proximal humeral physeal fractures: a matched cohort. J Pediatr Orthop. 2015;35:234-239.
- Liebs TR, Rompen I, Berger SM, et al. Health-related quality of life after conservatively and surgically-treated paediatric proximal humeral fractures. J Child Orthop. 2021;15:204-214.
- Gladstein AZ, Schade AT, Howard AW, et al. Reducing resource utilization during non-operative treatment of pediatric proximal humerus fractures. Orthop Traumatol Surg Res. 2017;103:115-118.
- Zuo J, Sano H, Yamamoto N, et al. Humeral head osteonecrosis in an adolescent amateur swimming athlete: a case report. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:39.
- Martin RP, Parsons DL. Avascular necrosis of the proximal humeral epiphysis after physeal fracture. A Case Report*. J Bone Joint Surg Am. 1997;79:760-762.
- Swarup I, Hughes MS, Bram JT, et al. Percutaneous pinning of pediatric proximal humeral fractures. JBJS Essent Surg Tech. 2019;9:e33.1-6.
- Rowles DJ, McGrory JE. Percutaneous pinning of the proximal part of the humerus. An anatomic study. J Bone Joint Surg Am. 2001;83:1695-1699.
- Zivanovic DV, Slavkovic AR, Radovanovic ZL, et al. Elastic stable intramedullary nailing of humerus fractures in children. Int J Clin Exp Med. 2018;11(4):2950-2964.
- Sénès FM, Catena N. Intramedullary osteosynthesis for metaphyseal and diaphyseal humeral fractures in developmental age. J Pediatr Orthop B. 2012;21:300-304.
