Original Research
Validation of a Novel Radiographic View for Evaluating Proximal Humerus Fractures: The Clear View
1Department of Orthopaedic Surgery, University of California San Diego, San Diego, CA; 2Division of Orthopedics, Rady Children’s Hospital and Health Center, San Diego, CA
Correspondence: Eric W. Edmonds, MD, Rady Children’s Hospital and Health Center, 3020 Children’s Way, MC 5054, San Diego, CA 92123. E-mail: [email protected]
Received: December 16, 2022; Accepted: May 5, 2023; Published: August 1, 2023
Volume 5, Number 3, August 2023
Abstract
Background: Orthogonal radiographs of the proximal humerus are challenging to obtain because the patient’s body mass can impede a quality lateral view and positioning of the shoulder can cause fracture displacement and patient discomfort. We describe a novel radiograph, the Clear View, taken 90 degrees to the scapular Y (SY), developed with the goal to minimize pain and reduce radiation exposure. We evaluate the ability to accurately assess proximal humerus fracture displacement utilizing the Clear View in comparison to the standard available x-rays and assess pain score when obtaining the Clear View.
Methods: Eleven independent observers at different levels of experience evaluated angulation and translation of three proximal humerus fractures: two cadaveric fractures and a third fracture in a 15-year-old to determine intra-observer correlation (ICC). Each fracture underwent the traditional radiographic series of anteroposterior (AP) in internal rotation (IR), AP in external rotation (ER), true axillary lateral (AX), SY, and transthoracic lateral (TRANS) plus computed tomography (CT). The Clear View was obtained on the two cadaver fractures. Pain scores based on the Wong-Baker FACES Pain Scale were assessed for individual radiographic projections in 13 patients with proximal humerus fractures.
Results: ICC was >0.6 for all measures. True fracture angulation was underestimated a majority (>75%) of the time in all radiographic views; TRANS (p<0.001) and AX (p<0.049) views had the least amount of error. Moreover, measures of translation were both underestimated and overestimated in all views, but the most accurate measures of translation were obtained with IR, ER, and Clear Views. Pain scores ranged from 0-1.2 when the Clear View was obtained.
Conclusions: Our study demonstrates that proximal humerus fracture angulation is often underestimated, and translation is difficult to measure regardless of view utilized. However, the Clear View, when combined with the AP view, offers an orthogonal, reproducible, valid measure of fracture translation and causes minimal patient discomfort.
Level of Evidence: Level II, prospective cohort study
Key Concepts
- Proximal humerus fracture angulation is often underestimated, and translation is difficult to measure regardless of view utilized.
- The newly described Clear View offers a reproducible, valid measure of fracture translation.
- The Clear View is associated with low patient discomfort.
- The Clear View may also reduce radiation exposure compared to standard transthoracic lateral imaging techniques.
- A combination of an AP and the Clear View is recommended as a reproducible and comfortable method to obtain orthogonal views with the ability to measure fracture angulation and translation.
Introduction
Quality orthogonal radiographs are required in order to appropriately evaluate fractures.1,2 The proximal humerus is unique in that a quality radiograph orthogonal to the AP is difficult to obtain due to the patient’s interposed thorax.3 In the adult literature, there has been significant evidence supporting the use of cross-sectional imaging to assess the displacement and fragment characteristics of each fracture but with limited success regarding reliability in assessment.2,4 In children, there is no evidence to justify the associated increased radiation exposure of obtaining CT scans, including when evaluating unicameral bone cysts, the most common cause of pathological fracture in this population, as radiographs have been shown to be adequate for diagnosis.5 Therefore, the assessment of the childhood proximal humerus fracture is centered on traditional radiographs.
Specialized lateral views are often limited by positioning restrictions due to pain and/or concern for further fracture displacement. Historically, the series of radiographs to view proximal humerus fractures include antero-posterior (AP) in internal rotation (IR), AP in external rotation (ER), axillary lateral (AX), Scapular Y lateral (SY), and/or Transthoracic lateral (TRANS) views.6,7 The AP internal rotation view tends to be the position of comfort for patients with proximal humerus fractures, as they cradle the forearm of the affected extremity across their body. However, movement of the fractured limb into the positions required to obtain the ER and the AX views can be painful and cause further displacement of the fracture. Moreover, the SY projection and TRANS views are suboptimal laterals given the SY is not orthogonal to the AP view, and it is difficult to visualize the proximal humerus through the entire chest and ribs on the TRANS view.
At our children’s hospital orthopaedic clinic and emergency department, we began obtaining an alternate view of the proximal humerus called the Clear View, which “clears” the thorax, reducing the radiation exposure necessary to penetrate the chest wall and achieving an image of diagnostic quality. The Clear View obtains an orthogonal projection from the medial side of the humerus (as opposed to the transthoracic lateral where the projection is obtained with beam penetration from the lateral side [Figure 1]). There is less concern for further fracture displacement since no positioning of the arm is imposed by the radiology technician. For the Clear View, patients merely lean forward and cradle their injured arm, avoiding external rotation or abduction of the shoulder required for ER and AX views. The purpose of this study was to evaluate the inter-rater reliability of the Clear View compared to the historical views of the proximal humerus to determine its ability to accurately assess fracture angulation and displacement and, secondarily, to assess pain scores when obtaining this view.
Figure 1. Clear View projection. Patient is upright with the affected humerus centered and in contact with the image receptor. The body is rotated 50 to 60 degrees toward the affected side until the humerus is clear of the chest, letting the arm swing out away from the chest. If not casted or splinted, the elbow is positioned comfortably flexed so that the contralateral hand may cradle or support the hand of the affected arm. Central ray is perpendicular to the midportion of the proximal humerus and center of the image receptor with a 40-48 inch focal-film distance.

Materials and Methods
Eleven observers (five pediatric orthopaedic surgeons, four pediatric orthopaedic fellows, and two orthopaedic surgery residents) were asked to evaluate angulation and translation of three proximal humerus fractures. The first fracture was in a 15-year-old male patient who sustained a proximal humerus fracture while playing football. This clinical case was selected for study, as there was a full set of high-quality standard radiographs along with a clinically uncommon, high-resolution computed tomography (CT) imaging exam. Two additional proximal humerus fractures were produced in a cadaver (76-year-old male deceased from lung cancer) with angulation and translation set using radiolucent foam wedges to represent in vivo fracture patterns. Inter-observer correlations (ICC) were determined for angulation and translation measurements on each traditional radiographic view by all 11 observers.
The institution’s traditional radiographic series of AP in IR, AP in ER, AX, SY, and TRANS views were obtained (Sedecal HF Series X-ray Generator, Madrid, Spain), and all identification markers were removed. The radiographic techniques matched the standard protocols utilized in our pediatric orthopaedic institution for imaging of the proximal humerus in a typical adolescent: AP in IR and in ER was 75kVp and 6.4 mAs, AX was 65kVp and 3.2 mAs, SY was 75kVp and 8 mAs, and TRANS was 90kVp and 40 mAs. Observers used angle and line measurement tools (Merge PACS™ [amipap02], Merge Healthcare Inc., Chicago, IL) to measure angulation (°) of the fracture and translation (mm) from each image.
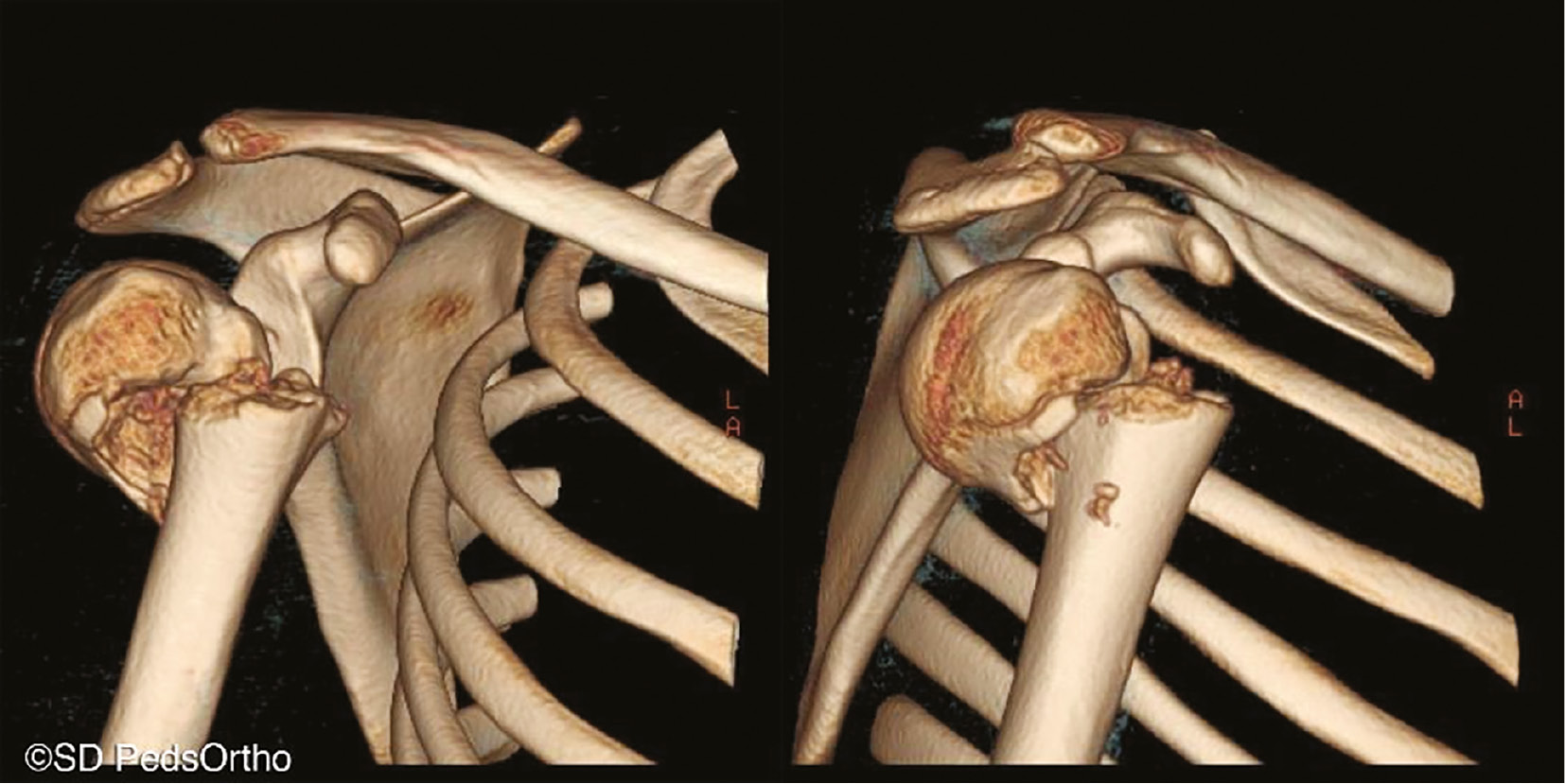
CT imaging (0.625 mm cuts, GE VCT 64-Slice LightSpeed CT Scanner, Piscataway, NJ) was obtained of the fractures, and 3D reconstructions were created (Mimics®, Materialise, Leuven, Belgium [Figure 2]). Three separate surgeons manipulated the 3D reconstructions within MergePACS™ to obtain the optimal view to assess true fracture angulation and translation. Their measurements were averaged to provide the true fracture angulation and translation.
Figure 2. 3D CT images manipulated to show anatomically true AP (on the left) and lateral (on the right) positioning of the proximal humerus.
The absolute difference between the true fracture angulation and translation from 3D CT measures and the measured angulation and translation from each radiographic view was calculated as the absolute error. Absolute error in measurements was compared amongst the traditional radiographic views using repeated measures ANOVA. Statistical significance was set at a critical alpha value of p<0.05 for all tests (SPSS Statistics, version 12, SPSS Inc., Chicago, IL).
Clear View radiographic projections for the two cadaveric proximal humerus fractures were obtained. The Clear View technique was set to be the same as the AP at 75kVp and 6.4 mAs since previous imaging has shown this technique provides adequate bony visualization, on par with the AP. Fracture angulation and translation were measured and compared to the true 3D measurements to assess the ICC and absolute error of this novel view.
To assess pain experienced with positioning for each view, data from a quality improvement initiative were reviewed. Pediatric patients with proximal humerus fractures within 3 weeks of the date of injury provided pain scores at the time of each radiographic projection based on the Wong-Baker FACES Pain Scale.8
Results
The ICC was greater than 0.6, moderate to excellent agreement according to Koo and Li,9 for all measures of angulation and translation (Table 1). As measured from 3D CT reconstructions, true fracture angulation and translation were as follows for the three fractures: Fracture 1 (15-year-old): 55.8±12.6°, 11.7±1.0mm; Fracture 2 (cadaveric): 49.0±4.3°, 8.5±1.4mm; Fracture 3 (cadaveric): 50.2±1.8°, 8.3±1.5mm. True fracture angulation was underestimated by a majority (>75%) of the observers in all radiographic views (Figure 3). However, measures of translation in IR, AX, and Clear View were equally underestimated and overestimated, while ER, SY, and TRANS led to underestimation (Figure 4). AX (p<0.049) and TRANS (p<0.001) views had less error in measuring angulation when compared to IR (Table 2). However, they had the most error compared to IR and ER when measuring translation. The most accurate measures of translation were obtained with IR, ER, and Clear Views.
Table 1.
| Angulation | Translation | |
|---|---|---|
| AP in IR | 0.760 | 0.641 |
| AP in ER | 0.913 | 0.870 |
| Axillary | 0.931 | 0.986 |
| Scapular Y | 0.984 | 0.975 |
| Transthoracic | 0.706 | 0.914 |
| Clear View | 0.712 | 0.945 |
Interobserver reliability ICC values, including 11 observers’ angulation and translation measurements of each radiographic view of the three fracture patterns studied (15-year-old and two cadaver fractures). Clear View ICC is of all 11 observers’ measurements of two fracture patterns in a cadaver.
Figure 3. Fracture angulation measured by 11 observers as over or under-estimation of actual angulation determined on 3D CT.
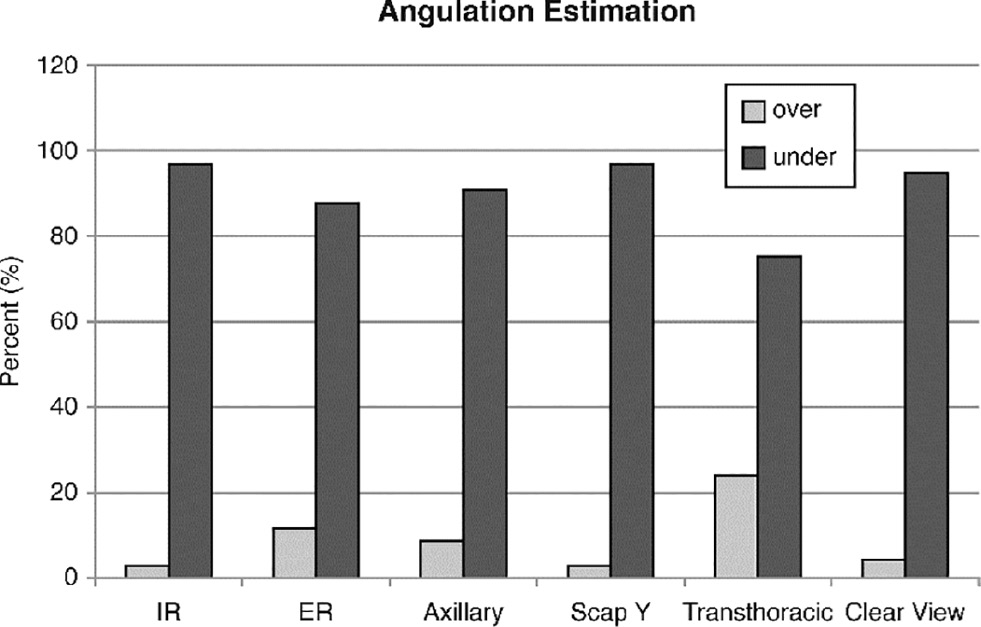
Figure 4. Fracture translation measured by 11 observers over or underestimation of actual translation determined on 3D CT.
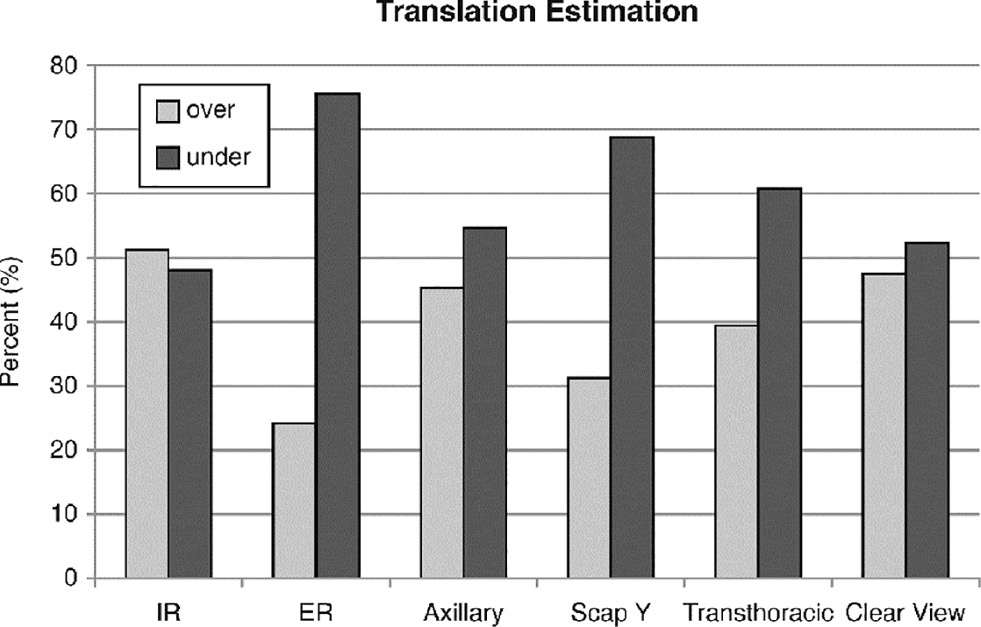
Table 2.
| Angulation (°) | Translation (mm) | |
|---|---|---|
| AP in IR | 40.8 ± 9.5 | 3.1 ± 2.3 |
| AP in ER | 29.4 ± 15.2 | 3.1 ± 2.4 |
| Axillary | 26.5 ± 18.1* | 7.7 ± 3.0#§ |
| Scapular Y | 31.1 ± 17.3 | 5.6 ± 3.3 |
| Transthoracic | 24.6 ± 14.9* | 9.6 ± 7.8# |
| Clear View | 35.5 ± 11.8 | 4.6 ± 2.1 |
Absolute error in measurements for fracture angulation and translation (values are mean ± standard deviation). *significantly less than AP in IR, # significantly more than ER and IR, § significantly more than Clear View.
Pain scores collected at the time of radiographic positioning were available for 13 children with proximal humerus fractures at a mean of 11.8 ± 4.9 days from the date of injury. The mean pain score with positioning for the Clear View was 0.12 ± 0.38, range 0 – 1.2. For example, one of the patients who had a near complete series of radiographs rated his pain as 2 on IR, 4 on ER, 0 on Clear View, and 3 on SY.
Discussion
Specialized radiographic views to assess fracture displacement and angulation are required for the treatment of pediatric proximal humerus fractures since CT is not often utilized.7,10–12 Historically, transthoracic lateral and AP views were thought to be the easiest and most comfortable method for achieving orthogonal images of these fractures. However, the reliability and validity of this method has not been studied even though axillary and scapular Y views13 have been shown to have poor reproducibility between raters and measures. Children typically tolerate displacement of proximal humerus fractures, and this has led to an acceptance of historical doctrine without trial.14 Our study demonstrates that fracture angulation is often underestimated and that translation is difficult to measure regardless of the view obtained. The radiographic Clear View offers improved utility compared to historical views in assessing displacement of proximal humerus fractures, providing a particularly useful view if the translation of the fracture is of high clinical concern, with less discomfort for the injured child, and potential for reduced radiation exposure.
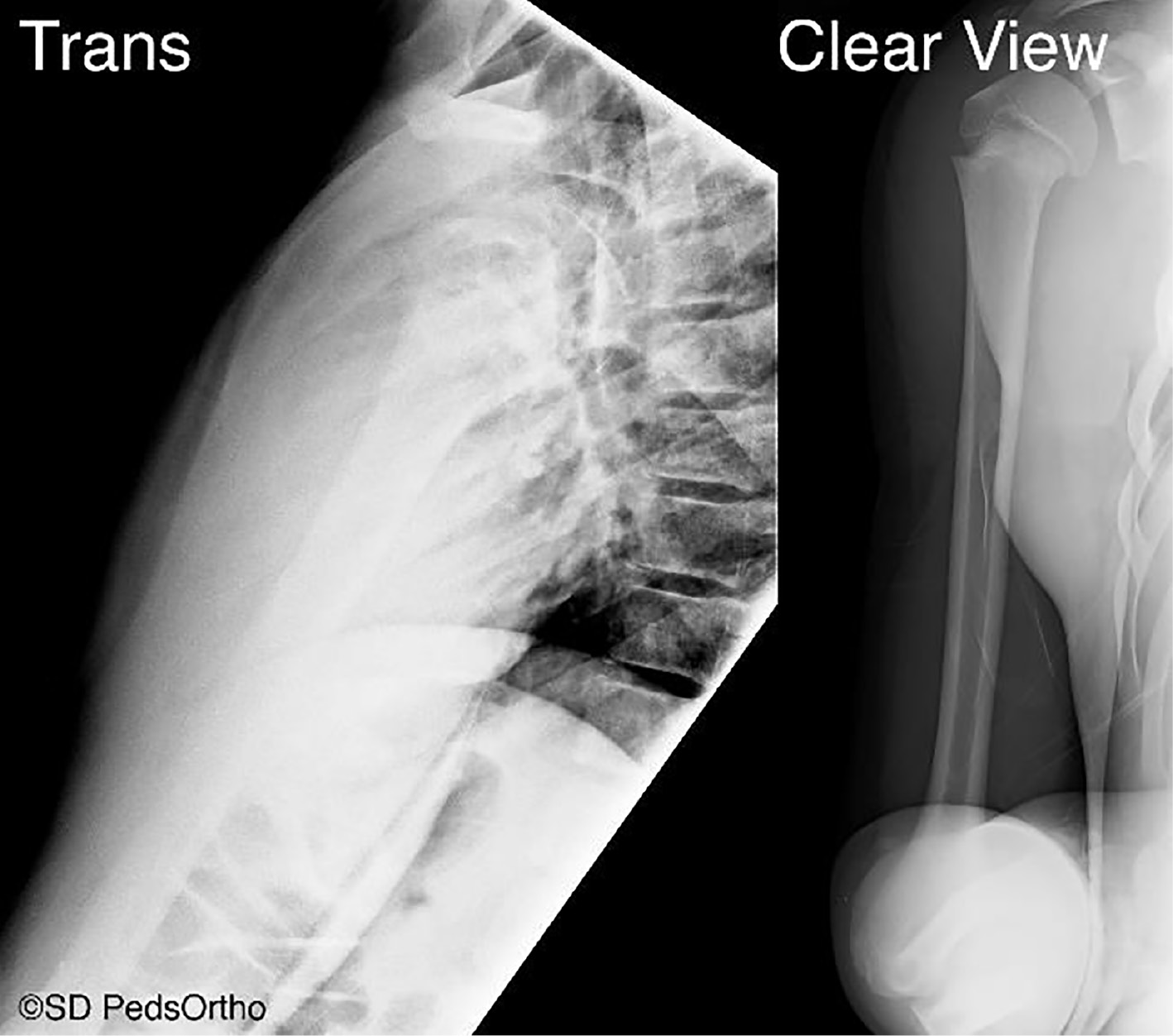
Our orthopaedic clinic lead radiology technician helped develop the Clear View to improve lateral visualization of the proximal humerus while also reducing the amount of radiation exposure required to penetrate the chest wall in a typical TRANS view of the humerus (Figure 5). Based on our institutional technique protocols, the TRANS had an equivalent radiation dose of 1.5 mSv versus 0.05 mSv for the AP and Clear View. The Clear View achieves a nearly orthogonal view to the standard AP image by having the child stand and lean forward slightly. Our institution follows “As Low As Reasonably Achievable” radiation principles when obtaining radiographs of children. Reducing radiation exposure is especially desirable in the pediatric population given their greater sensitivity to radiation with increased risk of acute lymphocytic leukemia and even fatal breast cancer from x-ray exposure.15 Although all current radiographic views of the shoulder expose the ipsilateral chest wall (and therefore breast tissue) to radiation, the Clear View reduces exposure risk compared to the TRANS view since less kVp and mAs are required to produce a diagnostic image. An orthogonal view to the Clear View is most often an AP in internal rotation as patients typically hold their injured arm against their body in this position for comfort.Therefore, these two views could be the basic radiographic set when assessing children with proximal humerus pain.
Figure 5. 12-year-old boy with proximal humerus fracture: Transthoracic view and Clear View taken in the same sitting. Both projections done without imposing rotation, thus minimizing discomfort for the patient. The Clear View uses less radiation while reliability of measurement (ICC in this study) is similar to transthoracic (Table 1).
The most significant limitation to this study is the utilization of an elderly cadaver to study a pediatric orthopaedic condition. CT scans are rarely obtained in pediatric proximal humerus fractures and pediatric cadaver specimens are difficult to acquire. The cadaver allows for CT and multiple radiographic imaging of the same specimen without harmful exposure to a patient. The small number of images reviewed by the observers is also a limitation, although this is partially countered by the fact that we utilized a larger number of observers. This study again highlights the inter-observer differences that can be seen between assessments of the historical specialized images of the shoulder.2,4
We propose the use of the Clear View to assess proximal humerus fractures. Its utility in evaluating the glenohumeral joint, however, is not validated. If clinical exam raises concern for shoulder dislocation, scapular Y or axillary views should be used as appropriately indicated. Additionally, there are patient-specific characteristics, such as large breasts, which could overlap with the fracture site and may require additional radiation exposure to obtain an image of diagnostic quality.
Patient age, fracture angulation, and displacement are key factors in determining operative versus nonoperative treatment of proximal humerus fractures.12,16 The findings of this study show significant differences between measurement modalities (Table 2), with conventional radiographs underestimating angulation while at the same time over- or under-estimating translation of proximal humerus fractures. While further study in the pediatric population is warranted to further optimize proximal humerus fracture imaging visualization while reducing radiation exposure, we propose the combination of an AP and the newly described Clear View (Figures 6 and 7). as a reproducible and comfortable method to obtain orthogonal views of the proximal humerus with the ability to measure fracture angulation and translation.
Figure 6. The Clear View can be helpful for very young patients. Radiographs of a 3-year-old boy demonstrating Clear View and AP in external rotation projections. These two views provide a reproducible method to obtain nearly orthogonal views with accurate measures of fracture translation and angulation.
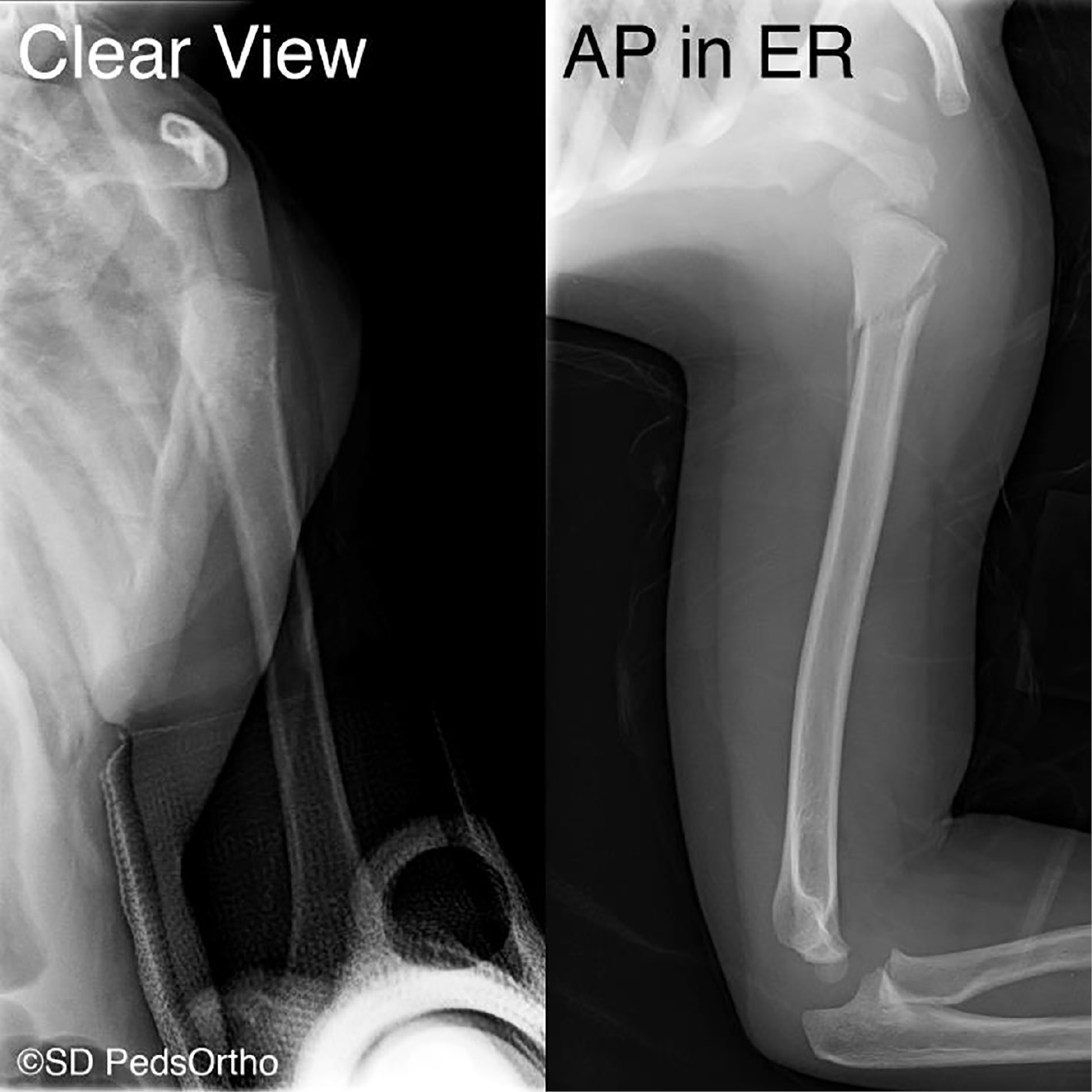
Figure 7. The Clear View also provides an adequate second projection option for adolescent patients. Radiographs of a 13-year-old boy with proximal humerus fracture Clear View and AP with internal and external rotation projections.

Acknowledgement
Tissue was supplied through an intramural grant from the University of California, San Diego Anatomical Materials Program. The authors would like to thank the 11 colleagues who provided x-ray assessments; James D. Bomar, MPH, for figure preparation; and Tracey P. Bastrom, MA, for statistical analysis.
Disclaimer
No funding was received. The authors report no conflicts of interest related to this manuscript.
References
- Sidor ML, Zuckerman JD, Lyon T, et al. Classification of proximal humerus fractures: the contribution of the scapular lateral and axillary radiographs. J Shoulder Elbow Surg. 1994;3(1):24-27.
- Bruinsma WE, Guitton TG, Warner JJ, et al. Interobserver reliability of classification and characterization of proximal humeral fractures: a comparison of two and three-dimensional CT. J Bone Joint Surg Am. 2013;95(17):1600-1604.
- Richardson JB, Ramsay A, Davidson JK, et al. Radiographs in shoulder trauma. J Bone Joint Surg Br. 1988;70(3):457-460.
- Sidor ML, Zuckerman JD, Lyon T, et al. The Neer classification system for proximal humeral fractures. An assessment of interobserver reliability and intraobserver reproducibility. J Bone Joint Surg Am. 1993;75(12):1745-1750.
- Mik G, Arkader A, Manteghi A, et al. Results of a minimally invasive technique for treatment of unicameral bone cysts. Clin Orthop Relat Res. 2009;467:2949-2954.
- Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077-1089.
- Kornguth PJ, Salazar AM. The apical oblique view of the shoulder: its usefulness in acute trauma. AJR Am J Roentgenol. 1987;149(1):113-116.
- Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17(1):50-54.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155-163.
- Dameron TB, Reibel DB. Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am. 1969;51(2):289-297.
- Shrader MW, Sanchez-Sotelo J, Sperling JW, et al. Understanding proximal humerus fractures: image analysis, classification, and treatment. J Shoulder Elbow Surg. 2005;14(5):497-505.
- Lefèvre Y, Journeau P, Angelliaume A, et al. Proximal humerus fractures in children and adolescents. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S149-S156.
- Siebenrock KA, Gerber C. The reproducibility of classification of fractures of the proximal end of the humerus. J Bone Joint Surg Am. 1993;75(12):1751-1755.
- Baxter MP, Wiley JJ. Fractures of the proximal humeral epiphysis. Their influence on humeral growth. J Bone Joint Surg Br. 1986;68(4):570-573.
- Willis CE, Slovis TL. The ALARA concept in pediatric CR and DR: dose reduction in pediatric radiographic exams--a white paper conference executive summary. Pediatr Radiol. 2004;34(Suppl 3):S162-S164.
- Popkin CA, Levine WN, Ahmad CS. Evaluation and management of pediatric proximal humerus fractures. J Am Acad Orthop Surg. 2015;23(2):77-86.
