Surgical/Technical Tips
Minimally Invasive Methods for Adolescent Intraarticular Distal Humerus Fractures with an Intact Column
1LSU Health New Orleans, Department of Orthopaedic Surgery, New Orleans, LA; 2University of Colorado, Department of Orthopedic Surgery, Aurora, CO
Correspondence: Austin J. Broussard, MD, LSU Health New Orleans, Department of Orthopaedic Surgery, 2021 Perdido St., 7th Floor, New Orleans, LA 70112. E-mail: [email protected]
Received: April 24, 2023; Accepted: June 15, 2023; Published: August 1, 2023
Volume 5, Number 3, August 2023
Abstract
Intraarticular distal humerus fractures can occur in adolescents and represent a unique morphology that is amenable to different surgical techniques than distal humerus fractures in adults or younger children, especially when one column remains intact. Despite articular involvement, a minimally invasive approach utilizing the intact periosteum and opposing intact column of bone can often achieve successful reduction and fixation. Here, we present operative techniques that we have found helpful for these fractures.
Key Concepts
- Intraarticular distal humerus fractures occur in adolescents and often demonstrate a characteristic pattern with a relatively vertical intraarticular fracture line with minimal articular comminution and limited displacement.
- Excellent reduction and fixation can often be accomplished through minimally invasive or percutaneous techniques, unlike most intraarticular distal humerus fractures in adults.
- In this paper, we describe straightforward fracture reduction methods, including indirect reduction via guide pins and cannulated screws alone or augmented with a periarticular clamp or ball-spike pusher.
- Our preferred fixation technique involves lateral-to-medial screws, ideally with one screw just proximal to the articular surface and additional screws as needed proximal to the olecranon fossa.
Introduction
Intraarticular distal humerus fractures in adults are usually bi-columnar injuries and are traditionally treated with open reduction and internal fixation, frequently through an olecranon osteotomy or triceps split.1,2 Medial and lateral plating is needed to connect the reduced and stabilized articular block to the humeral shaft. Adolescent patients often sustain intraarticular fractures of the distal humerus which are less extensive than those seen in adults. These are amenable to minimally invasive fixation; while they demonstrate intraarticular involvement akin to adult patients, they have less displacement and minimal comminution. These fractures variants can be more easily reduced (presumably due to robust periosteum) and can be stabilized to the intact column which obviates the need for plate fixation to the humeral shaft. The specific fracture morphology described here can often be treated with indirect reduction and percutaneous lag screw fixation. The purpose of this article is to present examples of this specific pattern of adolescent intraarticular distal humerus fractures and to describe technical tips for operative management unique to this pattern.
The electronic medical record of a tertiary academic pediatric hospital was reviewed to identify distal humerus fractures. From 2017 to 2022, 167 cases were identified. Of these, six cases met our criteria for inclusion: adolescent age group (12-16 years old), distal humerus fracture with intraarticular involvement, and at least one column of intact bone distally. Two cases were not included in this review due to plate and screw fixation and primary fracture involvement of medial epicondyle. The included fractures were minimally displaced, likely due to intact periosteum. CT scan images have been included for further illustration of these fracture types. These cases are presented here along with the operative techniques employed. Additional intraoperative reduction methods are also described with images to aid in this illustration.
Description of the Method
Lateral position with the patient’s arm over a bolster is well-described for distal humerus fractures in skeletally mature patients; we tend toward this positioning when there is bi-columnar instability and intraarticular comminution. In these cases, the patients should be intubated, and an axillary roll is placed with appropriate dependent padding. Prone positioning with the operative extremity over a bolster may also be used. At our institution, adolescent patients with less displaced uni-columnar fractures who are less likely to need plate fixation may be positioned supine with a radiolucent hand board attached to the operating table, potentially with laryngo-mask airway (LMA) technique depending on anesthesiologist preferences. A tourniquet is placed proximally on the operative extremity, which is prepped and draped in standard fashion.
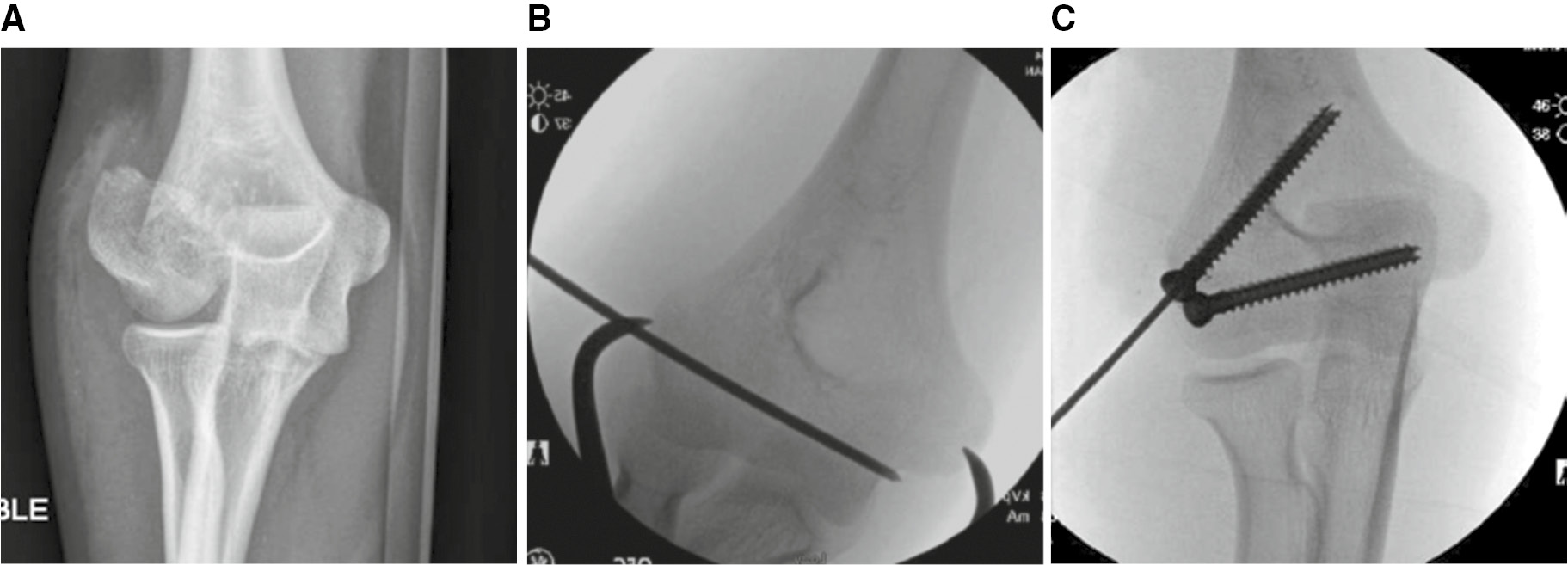
Reduction can be performed in a variety of methods. In some cases with minimal displacement, guide pins for cannulated screws are advanced across the fracture, and reduction is achieved by simple compression across partially threaded screws advanced over guide pins (Figure 1). In these cases, it’s important that the guide pins are placed parallel, as the fracture cannot be fully compressed when the pins are convergent or divergent. If guide pins are not perfectly parallel, the guide pins can be backed up to fracture site while one screw is advanced, and compression is achieved. It is best to advance the periarticular screw first to gain as much compression and congruity at the articular surface.
Figure 1. A case of an intraarticular distal humerus fracture in a 14-year-old male is shown in images A and B. The fracture was reduced using pins and then stabilized with partially threaded cannulated screws. Images C and D are follow-up radiographs obtained at approximately 4 months postop.

When parallel screw fixation and compression are not possible due to fracture configuration, an alternative technique to gain reduction and fixation is via a percutaneous clamp (Figure 2). In this case, the clamp is placed percutaneously and reduces and compresses the fracture prior to screw placement.
Figure 2. Image A demonstrates preoperative x-rays of a distal humerus fracture with one column intact. Images B and C are intraoperative fluoroscopy that demonstrate reduction of the joint surface using a pointed reduction clamp. After the periarticular screw is placed, the oblique screw provides metaphyseal support (Images courtesy of Kenneth Noonan, MD).
There is some risk to the ulnar nerve due to inadvertent placement of the tine of the clamp into the nerve or if the clamp should slip off posteriorly. This may be more likely in patients with significant swelling or in cases of obesity. In order to protect the ulnar nerve, it is wise to make a small incision and place a small temporary medial “safety screw” under direct vision which can very easily accommodate the clamp and will not displace (Figures 3–6).
Figure 3. This 14-year-old boy has a displaced distal humerus fracture of the medial column.

Figure 4. Through a small medial incision, a short screw is placed in the medial epicondyle under direct vision (A). The pointed reduction forceps easily engages the screw and cannot be displaced (B). Safe compression is effectuated, and the fracture is lagged in compression by over-drilling the near fragment with the 4.5 cannulated drill bit. The remainder of the procedure is completed, including removal of the short medial epicondyle screw (C-F).
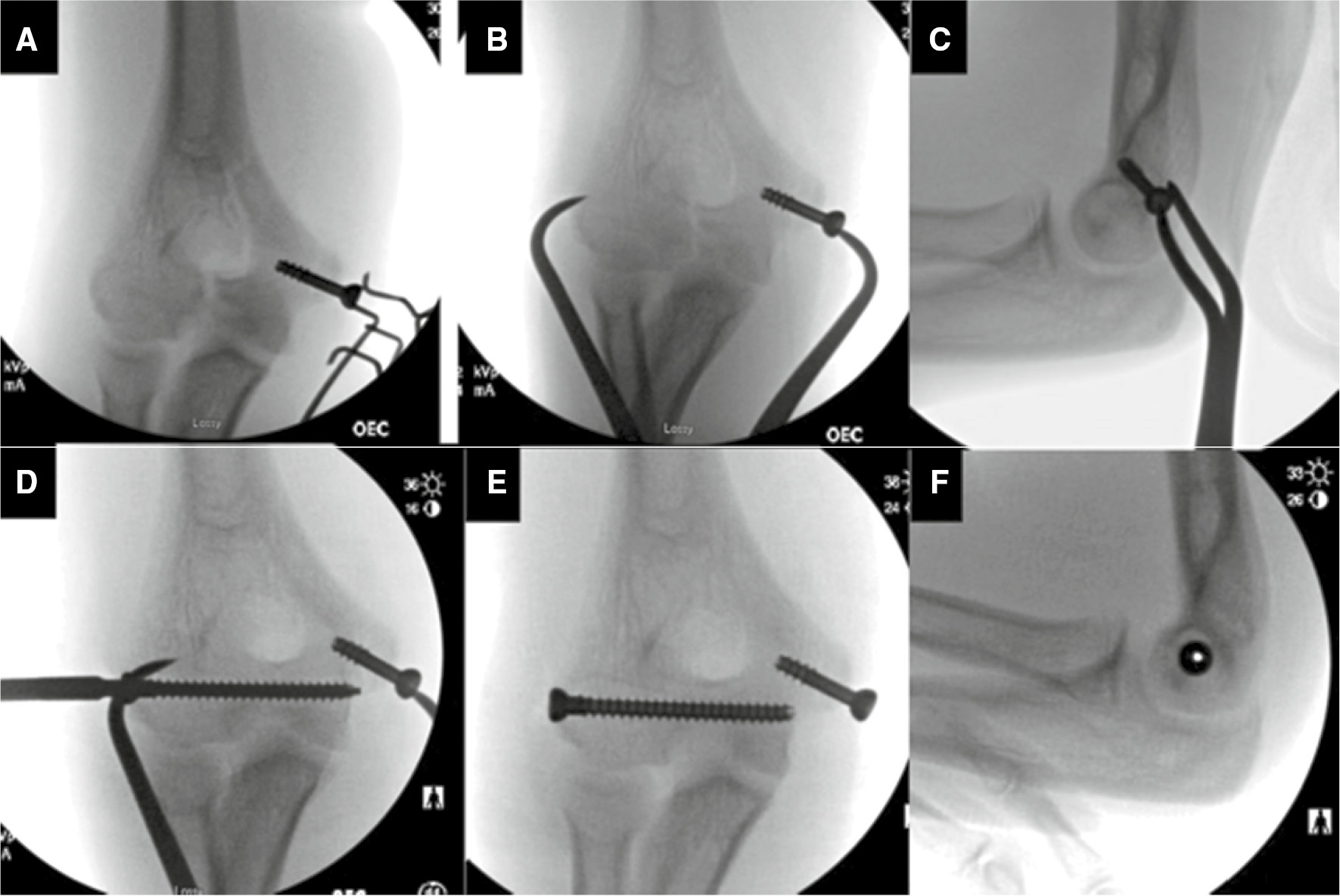
Figure 5. At one year follow-up, the fracture is healed, and the patient has full recovery and declined screw removal.

Figure 6. This 13-year-old girl has a displaced lateral column fracture treated with percutaneous reduction via a “medial safety screw.”
We have found the above technique works equally well for displaced lateral column fractures (Figure 6).
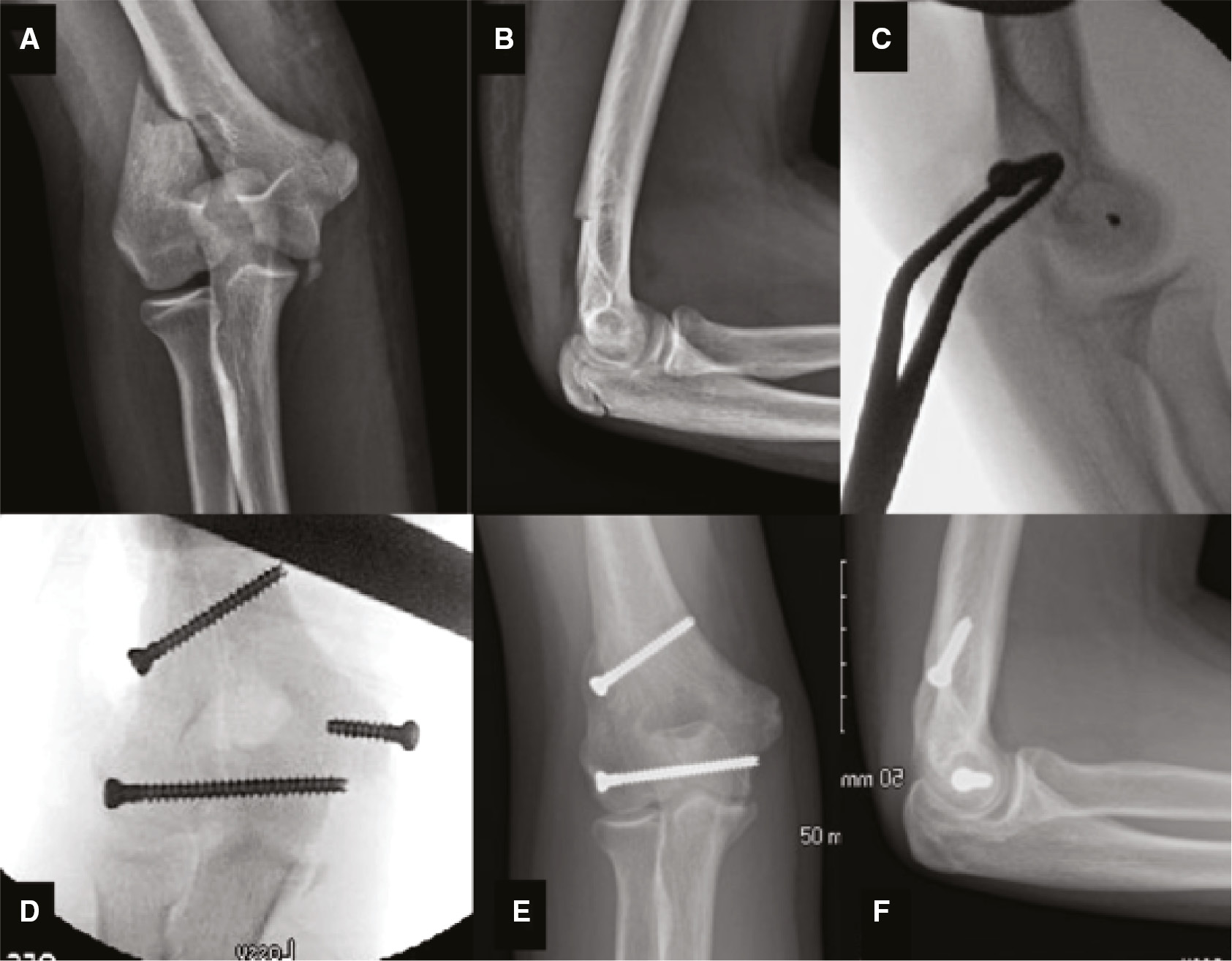
Another strategy to effectuate reduction involves using a periarticular reduction clamp with a folded towel over the medial side to protect the soft tissue (Figure 7). In another case, a periarticular reduction clamp was initially attempted but did not achieve anatomic reduction. A ball-spike pusher was then placed percutaneously through a small incision to apply lateral-to-medial force, which successfully maintained reduction while guide pins were advanced across the fracture, followed by partially threaded cannulated screws. Of note, all threads should cross the fracture line to ensure maximal compression and stability, particularly when spacing only allows for two screws (Figure 8).
Figure 7. Staged photo demonstrating periarticular reduction clamp technique with a folded towel between the medial tine and the medial epicondyle to protect the ulnar nerve. The lateral tine would be advanced directly to the cortex of the lateral condyle percutaneously through a 5 mm incision.

Figure 8. Images A and B are AP and lateral radiographs of a 12-year-old male taken at the time of injury, demonstrating an intraarticular distal humerus fracture that exits superior to the lateral condyle. Images C, D are AP and lateral x-rays taken 3 weeks postoperatively.

In addition to live fluoroscopic images, the joint may be further evaluated with an arthrogram (Figure 9). The arthrogram should be performed after fracture reduction and fixation; otherwise, dye leaking from the joint can obscure the imaging. The below case (Figure 9), like the one depicted above (Figures 3–5), demonstrates another important takeaway: lateral-to-medial screws can be used to successfully reduce a medial column fracture, even though most of the patterns we have encountered exited through the lateral column, which is intuitively more amenable to lateral-to- medial screw fixation. Again, care was taken in this case to ensure all threads crossed the fracture line.
Figure 9. Images A, B, C, D are x-rays and CT with 3D reconstruction images which show a 14-year-old male with left intraarticular distal humerus fracture. Images E, F, G are intraoperative fluoroscopy demonstrating three partially threaded cannulated screws oriented in a lateral to medial direction, Images F, G demonstrate lateral and AP intraoperative arthrogram following fixation.
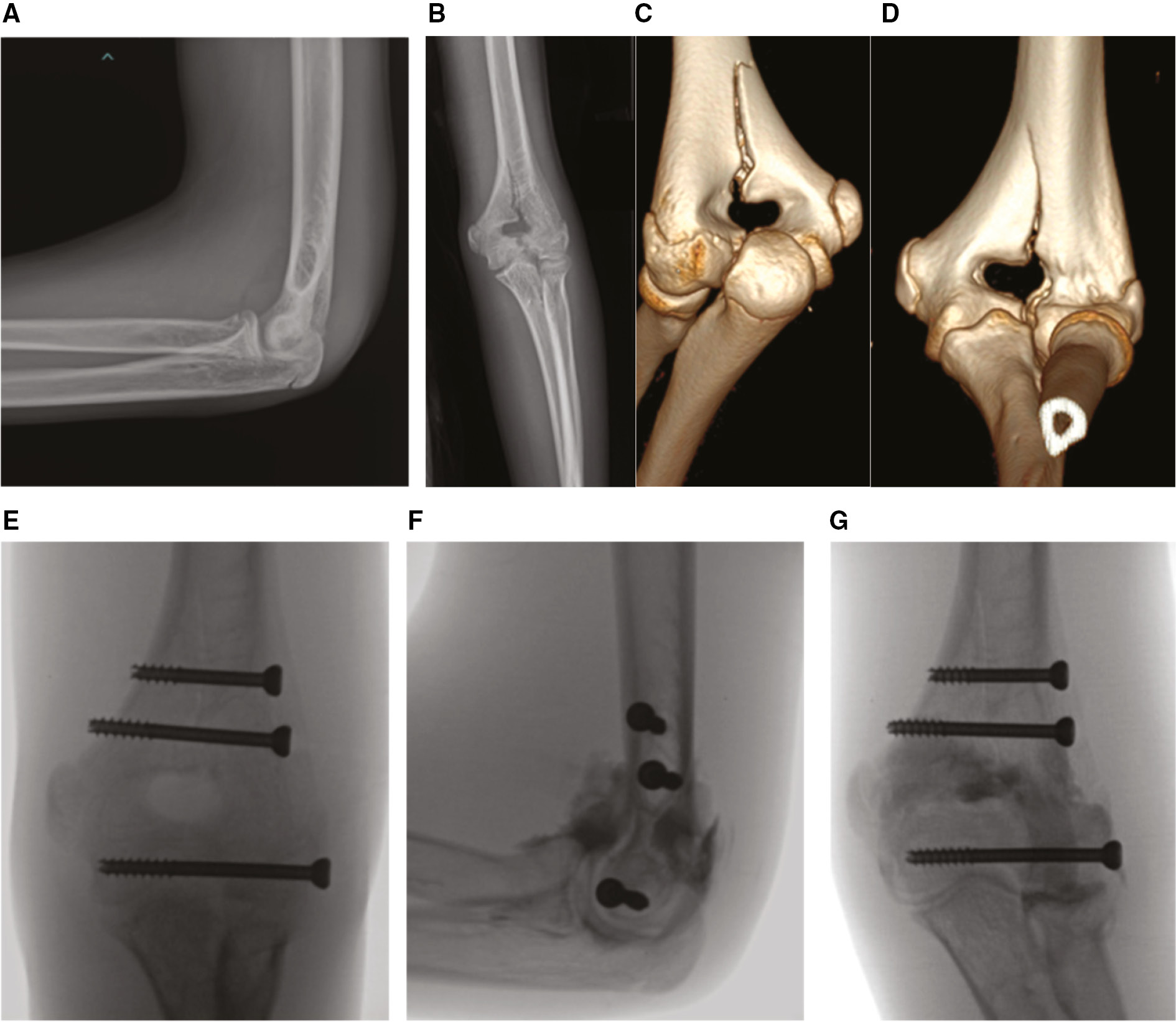
Finally, while this technique paper has focused on adolescent fracture patterns involving a single column, bi-columnar injury does not necessarily preclude closed reduction with minimally invasive screw fixation. In amenable bi-columnar fractures, the principles are the same: begin with closed reduction and a screw across the articular block to compress the joint surface. If sufficient space is not available above the olecranon fossa for a transverse screw, medial and lateral column screws can provide adequate stability (Figure 10).
Figure 10. Preoperative AP and lateral x-rays (A, B) and 3D CT reconstructions (C, D) demonstrating an adolescent supracondylar humerus fracture in a 12-year-old girl with an intraarticular split and extension through the lateral column and the majority of the medial column. This bicolumnar injury was successfully reduced and fixated percutaneously using cannulated screws, beginning with the articular block (E, F).

Postoperative Protocol and Results
Postoperative management varies between surgeons but usually includes a plaster splint or split (uni-valved or bi-valved) long arm fiberglass cast placed intraoperatively. Depending on fracture stability, some patients are converted to hinged braces at 1-2 weeks postoperatively. Patients are referred to physical therapy to work on range of motion and are instructed to avoid weight-bearing for 4-6 weeks and restricted from sports until healed with good functional motion. Routine follow-up is continued until the fracture is radiographically healed (usually within 3 months) and the patient has adequate motion. It is not uncommon for patients to ultimately lack 10-20 degrees of terminal extension.3
Discussion
Current literature on the operative management of intercondylar fractures in adolescents is sparse. Examples are typically represented in small case series,1,4 often including younger patients in the cohorts, which is problematic, as age likely contributes to fracture stability. Previous literature has described the management of T-type condylar fractures in adolescents2 and, more recently, a retrospective review of distal humerus fractures in adolescents captured 10 intraarticular AO classification B-type distal humerus fractures in adolescents.5 This group most closely resembles the cases illustrated here. Although their study does not explicitly describe the relatively vertical fracture morphologies presented here and they do not describe the same technique with transverse lag screws, the authors do credit closed reduction and percutaneous fixation of intraarticular injuries as a reasonable strategy.4,5
Safety of lateral-to-medial screws in the distal humerus has been described.6,7 Risks of this approach include injury to the radial nerve and intraarticular breach of implants. Based on cadaveric studies, there are two areas of safety for placement of hardware percutaneously in order to avoid injury to the radial nerve. The proximal safe zone exists from approximately 14.8 cm proximal to the lateral epicondyle to 5 cm distal to the acromion.6 However, the distal zone is the area of focus in this study. The traditional safe zone in adults, as described by Gerwin et al., is based on the finding that the radial nerve crosses the intermuscular septum approximately 10 cm proximal to the lateral epicondyle and then becomes an anterior structure.8 Arguably, a safe zone based on regional anatomy is more relevant than an absolute distance in children and adolescents where the anatomy is relatively smaller. Plucknette et al. described a lateral safe zone based on the transepicondylar width for external fixator pins, which is also very useful for placing percutaneous lag screws.6 Despite the relative safety of this distal zone, we still recommend avoiding “stab incisions” to protect underlying structures, including the radial nerve. Small skin incisions with careful blunt dissection may be employed for guide pin and screw placement as well as clamp placement if the fracture may not be compressed otherwise in a closed manner.
Our preferred construct is three screws with one screw within the articular spool, just proximal to the joint surface, and two screws proximal to the olecranon fossa. If the fracture line does not continue sufficiently proximal to allow for two screws proximal to the fossa, using only two screws may suffice. At least two of these screws should be partially threaded or lagged by technique to facilitate compression across the fracture. We recommend using cannulated screws, so reduction can be verified with guide pins in place before advancing the screws. If the reduction is in question, an arthrogram can be performed at this point. However, many of these patients are sufficiently skeletally mature to obviate the need for an arthrogram. Alternatively, intraoperative traction views may be helpful in assessing comminution at the articular surface, as this is poorly tolerated in the awake patient.9
The cases here all utilized screws with heads; however, headless screws could be used to reduce implant prominence, and thus, may improve postoperative motion. Postoperative elbow range of motion in these cases is consistent with current literature which suggests an expected loss of 15-30 degrees of motion.3 All patients discussed in this study lost between 10-20 degrees of extension. Despite similar outcomes between early motion and delayed motion protocols with regard to total arc of motion, Beck et al. demonstrated early postoperative mobilization decreased duration of stiffness with no adverse consequences in T-type condylar fractures in adolescents.10 Our patients are immobilized initially, with two transitioned to a brace at 2 weeks for early range of motion. We suggest implementing early motion protocols to optimize final elbow arc of motion. Other potential advantages of our suggested technique include shorter operative time, lower cost, and possibly lower incidence of hardware irritation and removal, especially if cannulated headless compression screws are used. This unique cohort of patients would benefit from larger, prospective studies to further investigate these advantages.
Conclusions
Intraarticular distal humerus fractures in adolescents behave differently than intraarticular fractures in adults, often displaying less displacement due to intact periosteum. In these fractures, minimally invasive fixation with percutaneous lag screws is a viable option for cases without articular comminution. This technique can provide adequate stability, early transition from immobilization post-operatively and avoidance of open plating techniques. The surgical technique is well-grounded in orthopaedic principles, including using periosteum to facilitate reduction in growing patients and favoring a less-invasive approach when possible.
Acknowledgements
The authors would like to thank Kenneth Noonan, MD, for providing supplementary imaging.
Additional Links
- POSNAcademy: Minimally Invasive Methods for Adolescent Intraarticular Distal Humerus Fractures
- POSNAcademy: Open Approach to Supracondylar Humerus Fractures
- POSNAcademy: Open Reduction and Percutaneous Pinning of Lateral Condyle Fracture
Disclaimer
No funding was received. The authors report no conflicts of interest related to this manuscript.
References
- Julfiqar M, Pabt A, Huda N, et al. Closed reductions and percutaneus ‘k’ wire fixation for adolescent intercondylar fractures of the distal humerus. J Clin Diagn Res. 2013;7(8):1666-1668.
- Re PR, Waters PM, Hresko T. T-condylar fractures of the distal humerus in children and adolescents. J Pediatr Orthop. 1999;19(3):313-318.
- Cook JB, Riccio AI, Anderson T, et al. Outcomes after surgical treatment of adolescent intra-articular distal humerus fractures. J Pediatr Orthop. 2016;36(8):773-779.
- Marengo L, Andreacchio A, Alberghina F, et al. Functional outcome of displaced intercondylar fractures of the humerus in children and adolescents. J Pediatr Orthop B. 2018;27(2):121-127.
- Bell P, Scannell BP, Loeffler BJ, et al. Adolescent distal humerus fractures: ORIF versus CRPP. J Pediatr Orthop. 2017;37(8):511-520.
- Plucknette BF, Tennent DJ, Hsu JR, et al. Lateral external-fixation adjacent to radial nerve. Cureus. 2020;12(3):e7435.
- Clement H, Pichler W, Tesch NP, et al. Anatomical basis of the risk of radial nerve injury related to the technique of external fixation applied to the distal humerus. Surg Radiol Anat. 2009;32(3):221-224.
- Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996;78(11):1690-1695.
- Popkin CA, Rosenwasser KA, Ellis HB Jr. Pediatric and adolescent T-type distal humerus fractures. J Am Acad Orthop Surg Glob Res Rev. 2017;1(8):e040.
- Beck NA, Ganley TJ, McKay S. et al. T-condylar fractures of the distal humerus in children: does early motion affect final range of motion? J Child Orthop. 2014;8:161-165.
