Historical Profile
Dr. Robert Bruce Salter: Memories from His Mentees
1Children’s Hospital of Eastern Ottawa, Ottawa, ON; 2UH Rainbow Babies & Children’s Hospital, Cleveland, OH; 3Foundation for Advancing Pediatric Orthopaedics, North Palm Beach, FL; 4Shriners Hospitals for Children–Portland, Portland, OR; 5AdventHealth West Florida, Tampa, FL; 6Shriners Hospitals for Children–Philadelphia, Philadelphia, PA
Correspondence: Sarah Nossov, MD, Shriners Hospitals for Children, 3551 North Broad St., Philadelphia, PA 19140. E-mail: [email protected]
Received: June 15, 2023; Accepted: June 27, 2023; Published: August 1, 2023
Volume 5, Number 3, August 2023
Introduction
An argument could be made that the most recognized name in the history of pediatric orthopaedics belongs to Dr. Robert Salter. Every medical student in the last 50 years has at least heard of his classification of growth plate injuries and most have been tested on it. His innovations and contributions to pediatric orthopaedics are numerous and have stood the test of time. In 2020, the Journal of Orthopaedics listed the most impactful pediatric orthopaedic literature, and Dr. Salter’s name is cited in 56 of the top 100 referenced papers.1
As time passes, the name and the impact made remain. Yet who was this man? What made him a legend and such an impactful figure? How did he educate, nurture, and raise the grandparents of our current pediatric orthopaedic family? The editorial staff is indebted to Drs. Heather Kong, Cheryl Lawing, and Sarah B. Nossov, from the POSNA History and Archives Committee, and to friends and colleagues Drs. Baxter Willis, George Thompson, and Peter Armstrong for shedding light on this remarkable man.
Dr. Salter circa 1977 (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
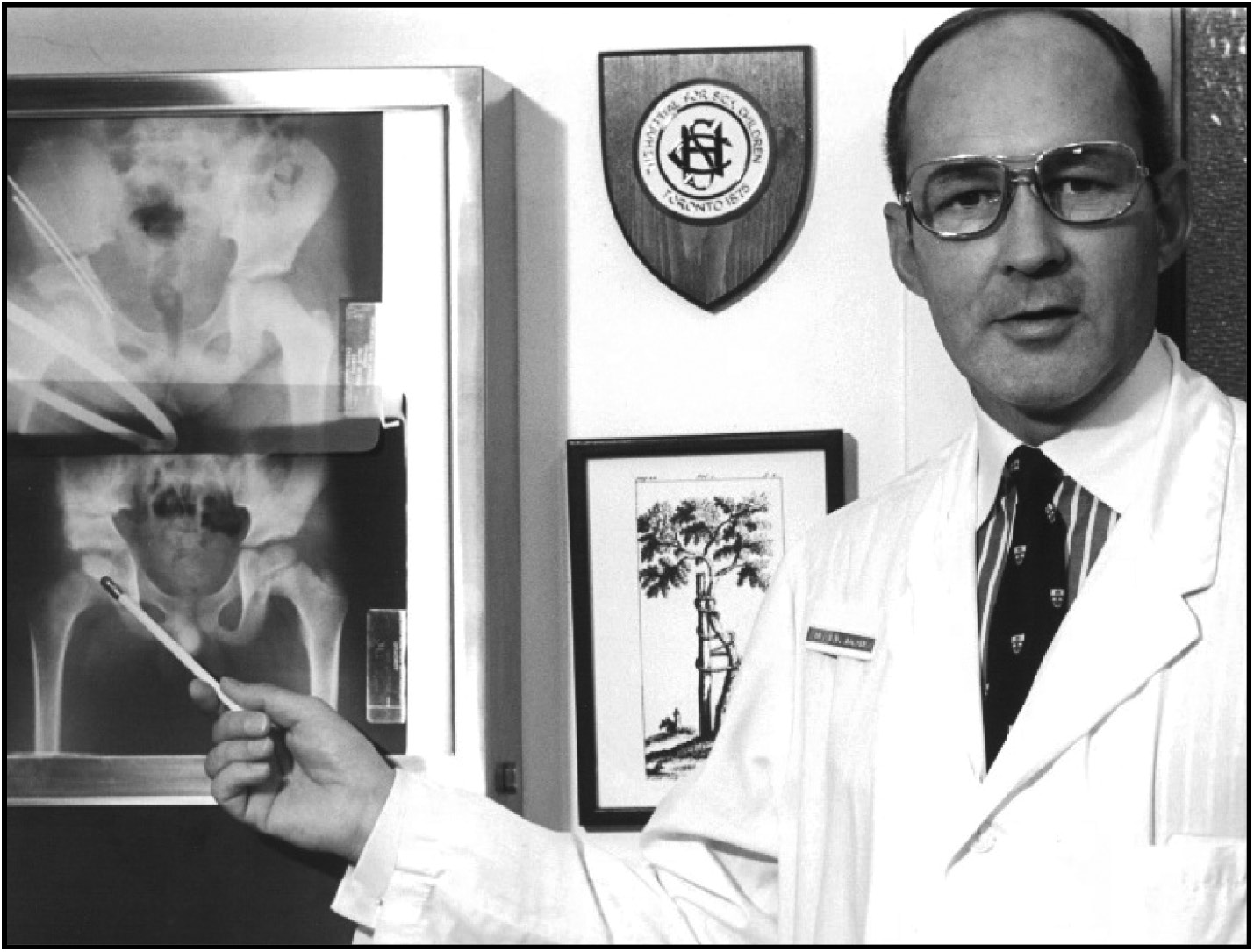
Dr. Salter circa 1973 (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
Baxter Willis, MD
Dr. Robert Bruce Salter was one of the giants of pediatric orthopaedics. His research into the management of developmental dislocation of the hip, the classification of growth plate fractures, and seminal work on the movement of joints after injury or surgery are some of the most critical advances in pediatric orthopaedics.
Training
Dr. Salter was born in 1924 in Stratford, Ontario, Canada, one of fraternal twins. He graduated from the Faculty of Medicine at the University of Toronto in 1947. He then spent 2 years at the Grenfell Medical Mission in Newfoundland & Labrador, followed by a surgical residency at the University of Toronto and a fellowship year at Oxford University in England as a McLaughlin Fellow. In 1955, he returned to Canada to join the medical staff at the Hospital for Sick Children (HSC). Two years after his appointment to the medical staff at HSC, he was appointed as the Chief of Orthopedic Surgery at the institution and subsequently became the Surgeon in Chief in 1966, a relatively meteoric rise in his professional career. He also attained the appointment of Professor and Head of the Division of Orthopedic Surgery at the University of Toronto and was elected President of both the Canadian Orthopaedic Association and the Royal College of Physicians and Surgeons of Canada.
Orthopaedic Contributions
Dr. Salter’s clinical contributions to pediatric orthopedics are enormous and start with his classification of growth plate injuries in partnership with Dr. Robert Harris in 1962.2 This classification is a modification of others but has stood the test of time and remains a classic, with particular emphasis on the location of the injury and eventual prognosis.
Dr. Salter always had an interest in Developmental Dysplasia of the hip (DDH–formerly Congenital Dislocation of the Hip–CDH), especially the anatomic changes with respect to the challenges of treating the child over 18 months of age. He showed that the acetabular volume in these children was similar to the uninvolved hip, but there was an acetabular mal-direction. If left untreated, this mal-direction makes open or closed reduction difficult to maintain. The “Salter osteotomy” (or “innominate osteotomy” as he preferred to call it), corrected the acetabular mal-direction by cutting the pelvis and rotating the distal fragment, including the acetabulum, through the symphysis pubis. After his classic article in 1961,3 the operation and his systematic treatment regimen for this complex condition became the standard of care, and long-term studies of hip patients have shown the results of this approach yielded excellent results.3 Soon after, he began to use the osteotomy as a means of “containing” the hip in patients with “head-at-risk” signs in the Legg-Calve-Perthes disease, with improved anterolateral coverage of the femoral head.
In the 1970s, Dr. Salter began a series of clinical experiments on rabbits to evaluate the concept of “continuous passive motion” (CPM) on the healing of articular cartilage injury and defects in the experimental animal. He showed that in intra-articular fractures and small articular cartilage defects, CPM could restore articular cartilage to virtually normal hyaline cartilage. This research led to the clinical adoption of CPM machines after surgery for joint injuries and reconstructions. He often thought of himself, or referred to himself, as “Bob the Mover” when presenting this research. The adoption of early motion after joint injury or surgery is universally accepted, and advances in our biomechanical understanding of the process are fueled by his original clinical research.
Dr. Salter at the SickKids Research Institute (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).

He always sought to ensure his audiences understood his message in clear, concise, and understandable language. At the same time, he could be a taskmaster for residents and fellows to accomplish the same goals during presentations at rounds and conferences. He ensured that English grammar and language were appropriate in discussions.
Salter’s approach to communication was exemplified by the Textbook of the Disorders and Injuries of the Musculoskeletal System, first published in 1971.4 For many medical students, this text was the introduction to fractures and diseases commonly seen in orthopaedic clinics. Written in a style that was eminently understandable by students, it inspired many to pursue a career in orthopaedic surgery.
Educational Contributions
One of Dr. Salter’s most significant accomplishments was the development of the clinical fellowship program, in conjunction with the world-class staff he was able to recruit to Toronto. The list of clinical fellows who trained at SickKids is legendary and includes Drs. Merv Letts, John Wedge, Vern Tolo, Dennis Wenger, Scott Mubarak, George Thompson, Peter Armstrong, and countless others whose influence in pediatric orthopaedics in the ensuing 30 to 40 years has been profound.
During the 1970s and 80s, SickKids was arguably the place to go for pediatric orthopaedic fellowship. This was, in large part, due to the experienced international faculty Dr. Salter had assembled with clinical expertise in virtually every area of subspecialty. The staff included Drs. Walter Bobechko (Spine), Donald Gibson (Spine, Muscular Dystrophy), Mercer Rang (Fractures, Neuromuscular Disease), Bob Gillespie (Spine, Tumours, Limb Deformity), Norris Carroll (Foot deformity, Fractures, and Complications), and Colin Moseley (Spine, Leg length Discrepancy, Hip Disorders). The strength of the staff is exemplified by the recruitment of several members of the staff to premiere U.S. institutions, including Norris Carroll to Children’s Memorial (Chicago), Bob Gillespie to Buffalo Children’s, and Colin Moseley to Shriners’ Hospital, Los Angeles. It was so strong, in fact, that Janet Walker, a former fellow in 1986-87, recalled an alum who explained to her that although they intended to work in arthroplasty, they came to SickKids to learn how to think.
Dr. Salter was a force to be reckoned with—in a positive way. Conferences and rounds were often contentious, with the staff often having different viewpoints on the management of a problem, but these disparate views served as an example of how an educational program could develop in a healthy and respectful manner even without consensus.
Dr. Salter had a few “trademarks” as well. He always wore shirts with a colorfulhonor body portion but always with a white collar. His ties usually repeated his interest in heraldry, often wearing the HSC tie with its coat of arms (which he developed) or the Royal College of Physicians & Surgeons of Canada tie, the organization of which he was President in 1977.
Dr. Salter with a resident in the SickKids Radiology Department, 1975 (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
Dr. Salter with Dr. John Wedge, shortly after Dr. Wedge became Chief of Surgery (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
Dr. Salter’s accomplishments in pediatric orthopaedics remain legendary. His legacy is celebrated frequently with a social or academic meeting of the Salter Society for graduated fellows of HSC.
Dr. Salter circa 1970s (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
I had the honor of being Dr. Salter’s clinical fellow in 1977, and I am grateful for his mentorship and personal friendship from 1977 until his passing.
George Thompson, MD
My year with Dr. Salter was in 1978 and was one of the most memorable times in my career. I first met him in 1976 when he was a visiting professor at UCLA Medical Center, and I was a PGY-4 resident assigned to assist him. I was able to discuss with him my interest in pediatric orthopaedic surgery. This began our 35-year relationship. It was further cemented when he accepted my invitation to visit our home for dinner when he was the guest speaker at the first international meeting on Legg-Calve-Perthes Disease in Los Angeles. I was also presenting my study from the Shriners Hospital for Children at that meeting. All these events culminated in being personally selected to be his fellow at HSC. My interview, as I remember it, was approximately 5 minutes in length. When I first arrived, he immediately asked that Dr. Donald Gibson come to his office. He informed him that I would be his fellow beginning the next January. The rest is history!
I have listed some of my memories but in no particular order. It is a given how much I learned from him with respect to pediatric orthopaedics, especially hip disorders. Perhaps most importantly, I learned the importance of interpersonal skills. He had an incredible way in how he dealt with medical students, residents, fellows, faculty members, and others, including nurses and employees. He was polite, courteous, and always had their best interest in mind. He kept personal information in his “black book” on spouse and children’s names, locations, institutions, and important points of information. While interacting with surgeons and visitors from other institutions or societies, he was always able to demonstrate his sincerity and interest by asking questions related to information in his book. (He always had sage advice and follow-through when necessary.) With parents and patients, he tried to establish a strong personal relationship. He lifted his patients onto the examination table even when it was a struggle with heavier patients. He always called his female patients “Duchess.” All this led to excellent doctor-parent/patient relationships and empathetic communications. He could explain clearly to patients their diagnosis, his recommendations, and discuss his current results with respect to the problem. In the operating room, he was a master technician. He always did the key components of any procedure but achieved an excellent but balanced approach with fellows and residents.
Dr. Salter (Chief of Surgery) and J. Douglas Snedden (Executive Director of SickKids) guiding Prime Minister Pierre Trudeau on a tour of the hospital in May 1971 (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
Research was another major strength. He had an inquisitive mind and an outstanding knowledge of the musculoskeletal system. He could recognize areas in need of clinical solutions and develop scientific ways to study them. He was also an outstanding writer and could communicate his findings in a clear, easy-to-understand way. This was another major strength in being his fellow. His scientific achievements brought him many national and international awards and accolades.
Following fellowship, we developed a deep professional relationship. He was always there to support me as my career progressed. It was this relationship that allowed me to work with HSC to help develop the Salter Society as a fellow alumni group. Unfortunately, my relationship let me observe his physical deterioration with advancing age. I am sure most of us remember receiving news of his passing while at the 2010 POSNA Annual Meeting in Hawaii.
Peter Armstrong, MD
I first met Dr. Salter in 1975. I was serving with the Canadian Forces in Lahr, West Germany, and had decided to apply for a residency position in the Toronto Orthopaedic Program. I was discussing going to Toronto for my interviews with a colleague who was a general surgeon at the base who had trained there. He told me that I would not see Dr. Salter as he was Chairman of the Division of Orthopaedic Surgery at the University of Toronto and would certainly not be interviewing resident candidates. When I got to Toronto, I was given my schedule, and the first name on the list was Dr. Robert Salter. Needless to say, I went in with trepidation to his office to meet and be interviewed by him. He immediately put me at ease, and we had a wonderful discussion. At the end, he said to me that he was not the only one who decides but that he was going to strongly recommend me for a residency position. I sort of floated out of the room!
It was during the 6-month rotation at SickKids that it became very clear to me that I wanted to be a pediatric orthopaedic surgeon. I was so impressed by the way he always showed incredible compassion to his patients and their families. He showed me that to be a pediatric orthopaedic surgeon, you obviously had to treat the child but also minister to the family.
Dr. Salter is pictured with the SickKids Coat of Arms, which he personally designed (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).
When I completed my residency, I applied to be a clinical fellow at SickKids and was overwhelmed when Dr. Salter selected me to be his fellow. It was a wonderful experience to be mentored by him. We had a great relationship throughout the fellowship. One very meaningful time was when we went to Sioux Lookout to do a clinic. At the end of the day, our flight back to Toronto was cancelled, and we had to stay overnight. We went out to dinner that night. During our conversation, he wanted me to call him Bob. I couldn’t bring myself to do that and chose to call him “Chief.” It was during that dinner that he told me that he wanted me to join the orthopaedic staff at SickKids. I was truly overwhelmed and didn’t know what to say other than “Thank you!”
One of the great experiences during my fellowship was to ride along in his Allard sports car. It was powered by a 331 cu in (5.4L) Cadillac engine, and to hear it “chortle” when he started it was something else. You had to sit on his raincoat on the passenger side, as someone had stolen the passenger seat. He liked to show me that if he was ever pulled over, he would open his wallet and just by coincidence, there was a button that showed his support of the Toronto Police Association. It was the first thing the officer saw before he pulled out his license.
One of his favorite quotes was that of Louis Pasteur who said, “When I look upon a child, I am filled with admiration for that child, not so much for what it is today, as for what it may become.” To this day, I still refer to that, as I believe it defines what we do and why we do it. We want to help children with orthopaedic disorders, and injuries maximize their potential “for what it may become.”
“Bob the Mover,” drawn by Dr. Salter’s colleague Dr. Mercer Rang. An inscription on the reverse reveals that this was gifted to Dr. Salter on December 15, 1980, by Dr. Rang, presumably as a birthday present (Photo courtesy Hospital Archives, The Hospital for Sick Children, Toronto).

Any of us who have spent a significant amount of time with Salter remember a number of what we might call “Salterisms.” One that I remember very well was when a resident was presenting a case and asked the faculty for their opinions on subsequent management. All of the faculty, with the exception of Dr. Salter, agreed on an approach. The resident turned to Dr. Salter and said, “Sir I think you are outvoted.” Without hesitation, Salter looked the resident right in the eye and said, “Son, I don’t count votes, I weigh them!” We all remember that he often called his innominate osteotomy the “No Name–No Fame osteotomy.” There are numerous others that are shared among those who spent focused time with him but, usually, not beyond that circle.
He was a great man, not perfect, but nonetheless great as a surgeon, a scientist, and, most of all, as a role model. I am so grateful that I had the opportunity to work with and learn from him as a resident, a fellow, and then a colleague. I am a better pediatric orthopaedic surgeon because of that opportunity.
*History and Archives Committee: Heather Kong, MD; Cheryl Lawing, MD; and Sarah B. Nossov, MD, edited this manuscript as members of the POSNA History and Archives Committee.
Acknowledgement
The authors would like to thank David Wencer, Archivist, The Hospital for Sick Children, Toronto, for the photos used throughout this manuscript.
Additional Links
POSNAcademy: Interview with Dr. Salter, 1996 POSNA Distinguished Achievement Award Winner
Disclaimer
No funding was received. The authors report no conflicts of interest related to this manuscript.
References
- Lum JC, Pereira GC, Giordani M, et al. Top 100 most cited articles in orthopaedic surgery: an update. J Orthop. 2020;19:132-137.
- Salter RB. Innominate osteotomy in the treatment of congenital dislocation & subluxation of the hip. J Bone Joint Surg Br. 1961;43-B(3):518-539.
- Salter RB, Harris WR. Injuries involving the growth plate. JBJS. 1962;45(3):587-622.
- Gulman B, Tuncay IC, Dabak N, et al. Salter’s innominate osteotomy in the treatment of congenital hip dislocation: a long-term review. J Pediatr Orthop. 1994;14(5):662-666.
- Salter RB. Textbook of Disorders and Injuries of the Musculoskeletal System: An Introduction to Orthopaedics, Fractures and Joint Injuries, Rheumatology. Philadelphia, PA; Williams & Wilkins; 1971.
