Current Concept Review
FDA Device Approval–What You Were Not Taught in Training
Tulane University School of Medicine, Children’s Hospital of New Orleans, New Orleans, LA
Correspondence: Timothy J. Skalak, MD, Children’s Hospital New Orleans, 200 Henry Clay Ave., New Orleans, LA 70118. E-mail: [email protected]
Received: August 5, 2023; Accepted: September 11, 2023; Published: November 15, 2023
Volume 5, Number 4, November 2023
Abstract
Medical devices are ubiquitous in the practice of pediatric orthopaedic surgery, but few surgeons receive any formal training or education on the process of bringing a medical device to market for pediatric orthopaedic patients. Innovation in the field of medical devices has led to significant improvement in the care of pediatric orthopaedic patients. The American Academy of Orthopaedic Surgeons (AAOS) and the Pediatric Orthopaedic Society of North America (POSNA) recognize the importance of making innovative medical devices available to pediatric patients and have made advocacy an important aspect of their mission and relationship with industry and governmental regulatory organizations.
Understanding the history, structure, and pathways to market approval are critical to encouraging the innovation of novel devices and techniques and improving the care of pediatric orthopaedic patients. Orthopaedists should have a command of the concepts of adverse event reporting as well as an understanding of the on- and off-label uses of medical devices as this is helpful for discussion of care and informed consent for the use of such devices.
Due to the relative rarity of the diseases addressed, pediatric orthopaedists should understand the framework of the humanitarian device exemption as well. These concepts can be synergized into some successful improvements in care for pediatric orthopaedic patients. One such success story in recent history was the introduction of the Vertical Expandable Titanium Prosthetic Rib (VEPTR) system by Dr. Robert Campell Jr.
Key Concepts
- The Food and Drug Administration (FDA) is the federal regulatory agency responsible for the approval and regulation of medical devices in the United States.
- The FDA classifies the risk of medical devices as low, medium, and high, and pathways to approval for devices vary based on this risk classification.
- One common exemption of importance to pediatric orthopaedic surgeons is the humanitarian device exemption, which can aid in the development and use of devices for the often relatively rare conditions faced by pediatric orthopaedic patients.
Introduction
The Food and Drug Administration (FDA) is the preeminent federal regulatory agency for the approval and regulation of medical devices in the United States.1 It has a wide variety of responsibilities, including therapeutic drugs used in both animals and humans, cosmetics, and medical devices, including orthopaedic implants. The FDA is an umbrella organization under the purview of the Department of Health and Human Services (HHS). As a regulatory body, it has six major roles in the regulation and surveillance of medical drugs and devices. These include:
- Marketing clearance and accurate labeling of medical products
- Alerting healthcare professionals of issues with products
- Removal of unsafe products from the market
- Monitoring importation and manufacture of products
- Regulation of clinical trials
- Post-market surveillance of drugs and devices
Brief History of Device Regulation
The inception of the Food and Drug Administration occurred in 1862 during the Lincoln administration with the passage of the Federal Food and Drug Act. The authority to regulate and oversee medical products was granted during the Roosevelt administration with the passage of the Federal Food, Drug, and Cosmetic Act (FD&C Act). Over the ensuing decades, with the significant proliferation of medical devices, the Cooper Committee was established during the Nixon administration in 1970. This committee introduced a risk-based classification for medical devices. Finally, device regulation specifically began with the Medical Device amendments to the FD&C Act on May 28, 1976. These amendments created the current three-class, risk-based classification system for all medical devices. It included any product that is used in a medical manner on humans ranging all the way from tongue depressors to lasers to novel orthopaedic devices. May 28, 1976, became foundational to the regulatory structure of the FDA, as any device not on the market prior to this date was subject to Premarket Approval.
The most recent evolution of this legislation is the Medical Device Fee and Modernization Act (MDUFA). MDUFA I was passed in 2002 in response to the FDA reports that underfunding was impeding the ability to perform timely reviews and permitted Congress to collect fees from the medical device industry, which now makes up roughly 35% of the FDA budget. The MDUFA underwent serial renewals with incremental changes and approaches its fifth renewal with MDUFA V passed in September 2022.
Relevant Structure to Orthopaedic Devices
There are six centers within the FDA of which the most relevant to orthopaedic device regulation is the Center for Devices and Radiological Health (CDRH), which regulates pre- and post-market surveillance.2 Within the CDRH are eight offices. The most relevant to the regulation of orthopaedic activities would be the Division of General, Restorative and Neurological Devices (DGRND). The activities of this office include reviewing requests to research and or market devices, collecting and analyzing information on injuries from devices, setting and enforcement of manufacturing practices, monitoring post-market compliance and surveillance, and assisting small manufacturers of devices. Fees collected include premarket, establishment registration fees, and product fees.
Classification and Pathways to Market for Devices
There exist three classifications established by the FDA for regulatory control of medical devices.3 These are stratified based on the relative increasing potential risk to the patient and are broadly classified as low, medium, and high-risk devices. Low-risk devices are mostly exempt from FDA notification and are subject to the fewest number of controls. Medium-risk devices can be exempt similar to low-risk devices if the device was on the market in 1976 or is “cleared” as equivalent to a legally marketed device at the time of the FD&C Act in 1976. All devices that were not on the market at the time of the passage of the medical device amendment are automatically classified as high-risk and are required to present clinical data to obtain approval for the market. These low-, medium-, and high-risk classifications therefore inform three different pathways to market for medical devices. An important distinction is that “cleared” and “approved” are not synonymous in the device regulation process and have differing requirements of scientific data for device marketing.
Class I – Low Risk
Class I or low-risk devices are generally subject to only general controls. Examples of Class I devices within the practice of orthopaedics include scalpels, saw blades, drills, and retractors. These controls include regulations to prevent mislabeling, registration of manufacturing facilities, as well as adverse event reporting to the Medical Device Adverse Event (MDR) system. Most Class I devices do not require a Premarket Notification 510(k), with the exception of a few, such as surgical gloves and skin staples.
Class II Medium Risk
Class II or medium-risk devices require premarket notification via the 510(k) process to the FDA. These devices require the general controls of Class I devices but also additional special controls specific to the device. Most orthopaedic implants fall within this classification, including plates, screws, intramedullary devices, spinal fixation implants as well as most joint replacement components. The specific controls required for these devices include post-market surveillance, patient registries, collection of clinical data as well as adherence to testing standards. Most Class I or Class II devices can trace their origins to a device in use prior to 1976, known as a predicate device.
Predicate Devices
A predicate device is either a device that was on the market prior to 1976 or a device that is legally marketed that has already been cleared for marketing as similar to an already cleared device.4 In order to meet this requirement, a premarket notification for a Class II device must provide data that shows it has the same intended use and same technological characteristics as a predicate device or has evidence to show the new device is as safe and effective as the predicate device. If the device is able to meet these requirements, the device is deemed to be substantially equivalent and is cleared for legal marketing.
Devices seeking clearance via similarity to a predicate device generally do not require clinical studies. They do, however, require preclinical testing that may include in vitro and in vivo safety testing, biocompatibility as well as product intended use labeling review. In some scenarios, a similar device may be being applied to a new or different population does require clinical data prior to clearance as substantially equivalent to a predicate device. An example of one such device within orthopaedics would be cervical pedicle screws.
Class III – High Risk
Devices falling into Class III, which includes all devices that are not Class I or II, require premarket approval. Premarket approval data must show reasonable assurance of the safety and effectiveness of the device. All devices not on the market in 1976 or able to be demonstrated to be equivalent to a predicate device fall into Class III. These devices present potentially unreasonable risk to the patient and therefore require the highest level of scrutiny, including clinical studies. These clinical trials are conducted under the Investigation of Device Exemption (IDE). This permits early patient access to novel devices in controlled settings after proof of concept is established. The IDE then provides the opportunity to provide evidence to establish the safety and effectiveness of a given device for an intended population with a specific intended use. Examples of Class III devices in orthopaedics include more novel devices such as vertebral disk replacements, mobile bearing total joint replacements, and hip resurfacing systems.
Exemptions
There are several important exemptions to the rigorous FDA approval process. First are the options for Humanitarian Device Exemption (HDE). Devices seeking an HDE are exempt from most user fees aside from establishment fees but still must meet criteria for effectiveness to obtain premarket approval. Another important exemption is made for small businesses with less than $30 million gross revenue and a partial exemption for those less than $100 million. The goal of such an exemption is to encourage small business development and innovation within the medical device space. Finally, the FDA may grant a waiver for any device felt to be substantially in the interest of public health in an emergency situation.
Adverse Event Reporting
Adverse event reporting is critical to the mission of safe device approval. This report must be timely and detailed. Reporting is important, as many initial safety studies may be small in number prior to the FDA approving the product for sale. Issues with products may only be discovered when it is used by a larger number of physicians or when a device use is extended to a population not studied in the initial clinical trials.5 Hospitals and surgical centers are required by law to report medical device-related mortality to the FDA as well as manufacturers.
On-Label vs. Off-Label Use
An important patient protection for medical devices is the proper labeling of medical devices. Labeling elements must be clear and understandable for patients. It must include all appropriate warnings, indications, and contraindications. All devices that are cleared or approved must have specific definitions for indications and intended use as well as terminology that describes the safe and effective use of the device. When a device is utilized for this specific labeled indication, the use is defined as “on-label.”
The FDA does recognize that medical practice and the best interests of the patient can potentially require the clinician to utilize a device outside the specific labeling parameters. This is defined as “off-label” or “physician-directed” use. It is incumbent upon the physician utilizing a device in this manner to use their professional judgment and be thoroughly informed of the specifics of the product and must reflect this use within the medical record. The manufacturer may not market the product for these uses, but the off-label use does not require an investigation drug application, investigational device exemption, or internal review board review. These reviews or applications are required if the use would be used to support expanded indication or change in the marketing of the device.
Physicians have the same prohibitions against the promotion of off-label use as companies. There are concerns about off-label use leading to inaccurate safety profiles for devices and potential incentives to diminish or eliminate the role of FDA approval for devices. In addition, without an evidence base, reimbursement for such off-label uses may not meet the CMS coverage determinations for insurance companies.
Challenges Facing Pediatric Orthopaedists
There are several challenges faced by pediatric orthopaedists in the development and implementation of devices for our patients. Pediatric orthopaedists take care of a very diverse and complicated patient population who may have pathology varying from the relatively common to the extremely rare. These inherent characteristics create roadblocks to bringing devices to market for patients.
First, the relative scarcity of some of these patients makes establishing criteria of efficacy and safety challenging to demonstrate to the FDA. The scarcity and heterogeneity inherent to the pediatric orthopaedic patient population present significant challenges to obtaining sufficient data to demonstrate efficacy and safety to the FDA. Further, the development of devices necessarily requires a partnership with industry for the development and implementation of devices. Naturally, medical device companies have a vested interest in profitability and return on investment for the research and development costs inherent to any device development. The pediatric population has lower rates of commercial insurance, which may affect reimbursement rates as well. Thus, in choosing the most effective allocation of resources, it certainly makes sense financially for companies to target diseases and devices that affect wider populations than those sometimes seen in the practice of a pediatric orthopaedist.
Second, perhaps the oldest aphorism in pediatric medicine is that “children are not just small adults.” This applies significantly to the development of devices. Children have different anatomy, often more active lifestyles, and of course, have significant changes in these and other parameters during development. Further, a child presents the possibility of longer-term device use, which may present longevity that may not be necessary in more adult-specific devices. Thus, when adult devices are borrowed for pediatric applications, they face challenges beyond what they may have been approved for by the FDA. Thus, the regulatory process intended to protect patients can at times pose extra barriers to the development of pediatric-specific devices.
Humanitarian Use Exemption
The FDA has created a pathway for device use in the many relatively rare conditions that may be present for evaluation by a pediatric orthopaedist. This is called a humanitarian use device and is governed by the humanitarian use exemption.6 A device may be eligible for humanitarian use if it is intended to benefit patients in the treatment of disease or diagnosis that affects 8000 or fewer patients in the United States per year. If a device meets that threshold, it can be exempt from the effectiveness requirements of the FD&C Act. The FDA Amendments Act of 2007 sought to enhance the availability and development of devices that were directed toward pediatric populations, defined by the FDA as age less than 22. This allowed for devices approved under the humanitarian use exemption to be sold for profit by companies if one of two conditions are met. First, the disease occurs in pediatric populations and the device is labeled for use in that population. Secondarily, the disease can occur in only adult patients or in such a way that development of a pediatric-specific device is impractical. The FDA also limits the number of Humanitarian Device Exemption devices that can be sold for profit, defined as the annual distribution number (ADN). The ADN is the number of reasonably needed devices per year multiplied by the target population; e.g., three devices needed per year with 7,000 patients would result in an AND of 21,000. For pediatric orthopaedists who care for many children with relatively uncommon diseases, this provides a pathway to develop devices for those patients as well as a pathway for industry to recoup their investment in such device development.
Dr. Robert Campell Jr. (1951-2018) VEPTR, a Pediatric Device Success Story
One remarkable relatively recent example of pediatric device development was Robert Campell Jr., MD (Figure 1A). His work in San Antonio and later Philadelphia revolutionized the care of children with severe spinal and chest wall deformities. The Vertical Expandable Prosthetic Titanium Rib (VEPTR) system was initially based on a Steinman pin chest wall prosthesis.7 In a prototypical form, it was inserted in an 8-month-old ventilator-dependent child in San Antonio in 1987. To the surprise of many involved in the child’s care, the child was weaned off the ventilator and eventually off oxygen in the postoperative period. Now that the child appeared hopeful to survive and continue to grow, the non-expansile Steinman pin construct now presented a tether to spinal and thoracic growth and development. Dr. Cambell was left with two choices: either subject the child to repeated full thoracotomy and removal and reimplantation of the device or work to develop a thoracic wall-specific prosthesis that could be expanded and potentially reduce the morbidity to a fragile patient population. He chose that latter course with the problem being at the time that such a device did not exist.
Figure 1A. Robert Campell Jr., MD, 1951-2018. Dr. Campbell’s work revolutionized the care of children with severe spinal and chest wall deformities.

Thus, Dr. Cambell began searching for a manufacturer both willing and capable of making such a novel device. At the time, no surgical manufacturer had a chest wall prosthesis that seemed possible to make expandable, so Dr. Campell consulted with orthopaedic manufacturers. As one might expect, the significant technical challenges of such a device as well as at the time a market of a single patient did not attract a lot of interest from industry partners. Eventually, a custom orthopaedic manufacturer (Techmedica, Camarillo, CA, USA) agreed to make a custom titanium alloy rib which was first placed in April of 1989. The success of this procedure resulted in significant global referrals of diverse and heterogeneous patients, which eventually led to the development of the diagnosis we now know as thoracic insufficiency syndrome. In partnership with Dr. Melvin Smith, a pediatric surgeon, they developed new devices and surgical procedures for its application.
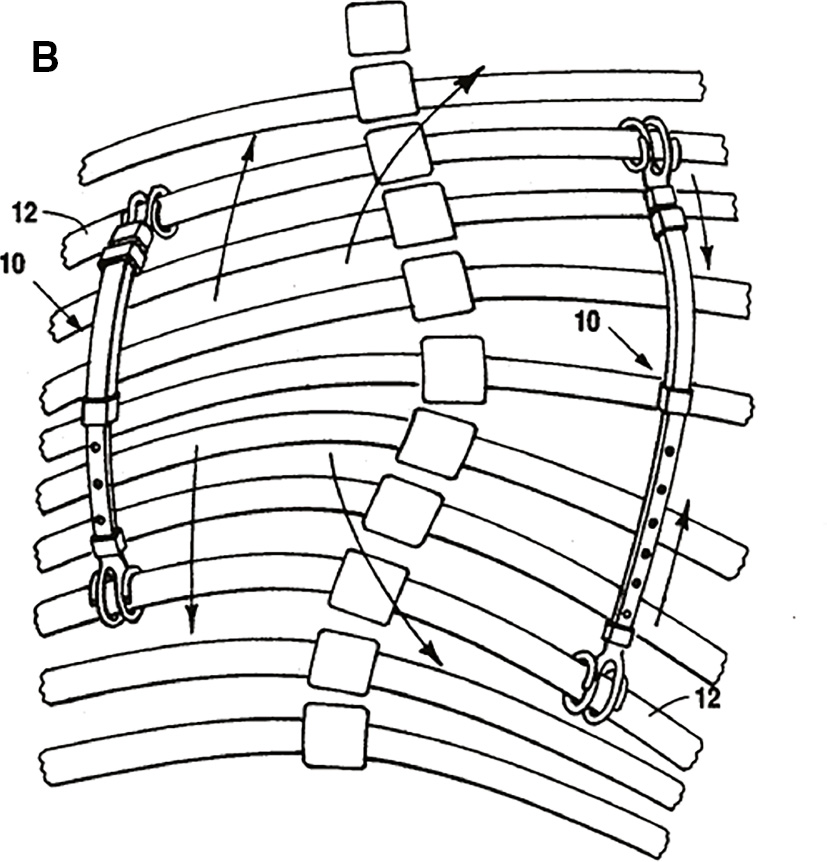
The journey to approval in the U.S. was far from over, however. Indeed, only in 2004, after one of the lengthiest approval processes in U.S. history, was VEPTR approved under a humanitarian device exemption (Figure 1B). From 1992-1994 a sole site FDA feasibility study occurred in San Antonio. Subsequently, Synthes Spine (Westchester, PA) assumed device development of the VEPTR and sought to expand its application beyond the results in San Antonio. Fortunately, the success was repeatable in diverse locales around the country. With sponsorship from industry partners, training was made available as well as travel sponsorship for pioneering surgeons to travel and mentor other surgeons adopting the VEPTR into their practice. The VEPTR device has gained wide acceptance for application in thoracic insufficiency and is now in use in over 26 countries around the world. Dr. Campell’s story is an inspiring example of how a pediatric orthopaedist, with an extensive team of medical and industry partners, can create a device that revolutionizes the care of patients around the world.
Involvement of the AAOS/POSNA
The American Academy of Orthopaedic Surgeons plays a role in the device approval process via the Orthopaedic and Rehabilitation Devices Advisory Panel. This panel advises the FDA regarding approval or reclassification of devices as well as appropriate testing protocols. In addition, the AAOS Exhibits Committee works with the FDA at the annual meeting to ensure correct disclaimers in both educational courses as well as vendor product displays. Within POSNA itself, the Advocacy Committee has been working with our AAOS lobbyist to promote pediatric device approval as well as advocating for the approval of MDUFA V.
Summary
Medical devices are intrinsic to the practice of pediatric orthopaedic surgery. Innovation and improvement in pediatric orthopaedic devices have inarguably improved the care for patients undergoing treatment for a wide variety of pediatric orthopaedic conditions. The Food and Drug Administration (FDA) stratifies the risks associated with medical devices and governs the pathways to approval. Off-label use and the humanitarian device exemption provide two alternative ways for pediatric orthopaedists to be able to provide access to medical devices for patients. The partnership between astute physicians and industry partners can lead to the availability of novel devices for children with rare diseases such as the introduction of the VEPTR by Dr. Campell. It is critical for surgeons and our organizations to have an understanding of the device approval process so that we can maximize the care and innovation available to our patients.
Acknowledgements
*The author wishes to acknowledge Kali Tileston, MD; Kerwyn Jones, MD; Rebecca Clinton, MD; Timothy C. Borden, MD; Folorunsho Edobor-Osula, MD; David Fralinger, MD; Grant D. Hogue, MD; Michelle Mo, MD; Samantha Spencer, MD; and Amanda T. Whitaker, MD, from the POSNA Advocacy Committee, for the conceptualization, content evaluation, and critical feedback with the development of this current concept review.
Disclaimer
The author reports no conflicts of interest related to this manuscript.
Additional Links
- U.S. Food & Drug Administration: Devices Approvals, Denials and Clearances
- Congressional Research Service Reports
- U.S. Food & Drug Administration: Humanitarian Device Exemption
References
- Federal Food, Drug, and Cosmetic Act (FD&C Act). United States Code (U.S.C.) Title 21, Chapter 9.
- Sastry A. Overview of the US FDA medical device approval process. Curr Cardiol Rep. 2014;16:1-5.
- Darrow JJ, Avorn J, Kesselheim AS. FDA regulation and approval of medical devices: 1976-2020. JAMA. 2021;326(5):420-432.
- Buch B. FDA medical device approval: things you didn’t learn in medical school or residency. Am J Orthop (Belle Mead NJ). 2007;36(8):407-412.
- Dubin JR, Enriquez JR, Cheng AL, et al. Risk of recall associated with modifications to high-risk medical devices approved through US food and drug administration supplements. JAMA Netw Open. 2023;6(4):e237699-e237699.
- Bernad DM. Humanitarian use device and humanitarian device exemption regulatory programs: pros and cons. Expert Rev Med Dev. 2009;6(2):137-145.
- Campbell RM. VEPTR: past experience and the future of VEPTR principles. Eur Spine J. 2016;22:106-117.