Original Research
Evaluating the Etiology of Osteochondritis Dissecans of the Knee: The Role of the Articular-Epiphyseal Cartilage Complex
1Department of Orthopaedic Surgery, University of California – San Diego, San Diego, CA; 2Division of Orthopaedic Surgery, Rady Children’s Hospital, San Diego, CA; 3Department of Orthopedics – University of Minnesota, Minneapolis, MN
Correspondence: Eric W. Edmonds, MD, Rady Children’s Hospital, San Diego, 3020 Children’s Way, MC 5054, San Diego, CA 92123. E-mail: [email protected]
Received: February 23, 2023; Accepted: July 27, 2023; Published: November 15, 2023
Volume 5, Number 4, November 2023
Abstract
Introduction: In pathologic form, osteochondritis dissecans (OCD) is a focal end-stage disease of articular cartilage. Comparative anatomy studies have demonstrated that injury to epiphyseal anlage cartilage leads to development of OCD in many species, whereas in humans, the exact etiology is suspected but remains unknown. A potential candidate is the articular-epiphyseal cartilage complex, and our hypothesis is that injury at the junction between the epiphyseal anlage cartilage and the articular cartilage results in childhood OCD.
Methods: A retrospective, two-institution assessment of children with magnetic resonance imaging (MRI) of the affected knee before the onset of an OCD lesion was performed. Demographics were recorded, including the history of why each initial pre-OCD MRI (Index-MRI) was obtained. MRI measurements were made on the Index-MRI as well as the subsequent OCD-MRI of the epiphyseal ossification length (Growth), marrow edema, the distance of lesion from physis (Lesion Position), and the distance from articular surface (OCD Depth). Comparisons over time were then calculated.
Results: Six children (seven knees) were identified with an Index-MRI (Pre-OCD development) obtained at median age 11.6 years and OCD-MRI obtained at a median of 1.9 years later. ‘Growth’ occurred in at least one dimension for all children (sagittal MRI, p=0.018). As a group, the ‘Lesion Position’ did not change significantly in any plane but two demonstrated continued ossification of the epiphysis and one demonstrated bone necrosis. As a group, the ‘OCD Depth’ was significantly different (coronal plane, p=0.029 and sagittal plane, p=0.026) over time, with all lesions increasing their depth (since none existed on the Index-MRI).
Discussion: Even though the articular-epiphyseal cartilage complex appeared to be involved with the etiology of knee OCD in this limited series, we found significant variation in the response to a presumed injury with either halted progression, continued ossification, or even regression of ossification adjacent to the OCD. This variation either indicates that there is a multimodal etiology, or that the articular-epiphyseal cartilage complex inconsistently responds to injury. This may explain the inconsistent response to management and calls for further basic science studies to ascertain the exact location of injury in the human articular-epiphyseal cartilage complex.
Level of Evidence: III, Retrospective Cohort Study
Key Concepts
- Osteochondritis dissecans may have more than one etiology that leads to a similar pathology pattern at the time of presentation.
- Future study will be important to identify when certain patterns of progression are present that may indicate one management modality over another one.
- Understanding the variation in OCD etiology may have repercussions regarding animal model development.
Introduction
Osteochondritis dissecans (OCD) has been defined in the orthopaedic literature as a focal, idiopathic alteration of subchondral bone with risk for instability and disruption of adjacent articular cartilage that may result in premature osteoarthritis.1 This definition was created from the body of evidence in human-based literature. König first coined the term in 1888 describing the creation of loose bodies in a joint in the absence of trauma.2 Ischemia has long been postulated as a possible cause of osteochondrosis.3,4 Genetic predisposition has also been established as a possible cause with growing evidence of involved loci.5–8 Repetitive microtrauma has been well-established as another potential contributor to OCD, given the high incidence of these injuries in the athletic population.9–11 Comparative anatomy studies in pigs, goats, and horses, as well as radiographic studies in humans, now indicate a direct causal relationship between the development of OCD and loss of blood supply (due to water-shedding of vascularity) to the anlage cartilage of the epiphyseal bone (Figure 1); however, there is no evidence that this pathologic process in animals, which appears similar to human OCD, is indeed the same pathologic process seen in children.12–15
Figure 1. Distal femoral epiphysis of a 3-week-old piglet, demonstrating the cartilage canal blood vessels throughout the anlage cartilage of the epiphysis (circle), dark center is secondary ossification center, and the arrowheads denote the location of the ossification front. Note the absence of vascularity at the articular cartilage (arrow). The entirety of the junction between the ossification front and the junction between the avascular and vascular cartilage is considered the articular-epiphyseal cartilage complex for the purposes of this study.

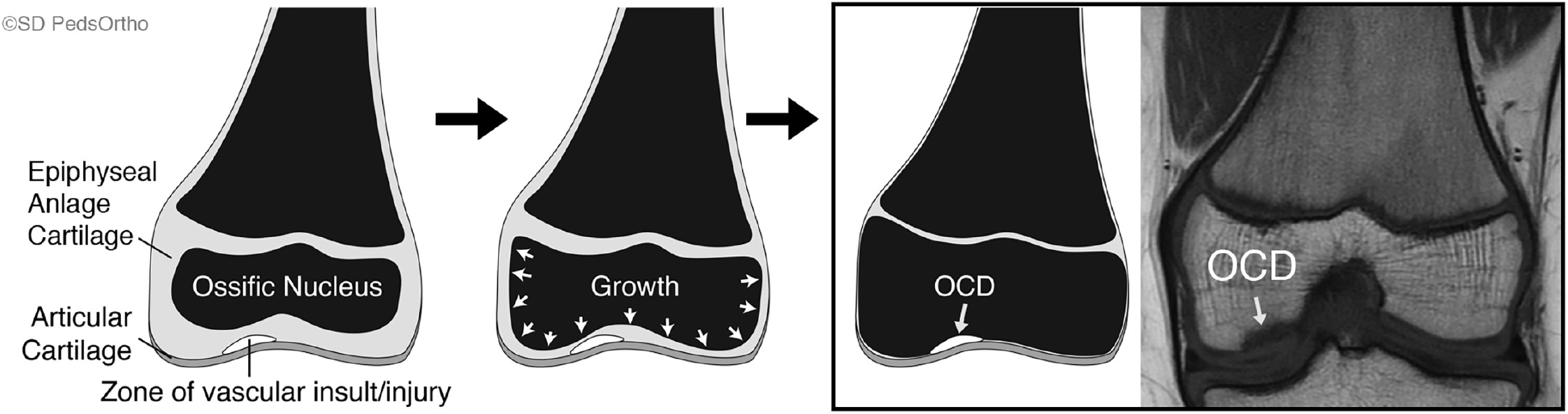
The anlage cartilage of epiphyseal bone is ossified by a secondary physis that serves to enlarge the epiphyseal center of ossification via circumferential growth that mirrors the shape of the epiphysis. It is responsible for bone growth by endochondral ossification and for maintaining the shape of the articular surface.16 This articular-epiphyseal cartilage complex undergoes, as of yet, a not fully understood maturation process that entails both appositional and interstitial growth in symphony with cell apoptosis, proliferation, as well as matrix resorption and mineralization.17,18 Endochondral ossification is heavily influenced by mechanical loading and biological factors.19 It has been shown in rabbits that mechanical compressive stresses can lower bone growth rates.20 Magnetic resonance imaging (MRI) studies in animals have revealed disruption of the physis with both metaphyseal and epiphyseal injury.21,22 Physeal widening has also been noted in the perigenicular growth plates of child athletes involved in contact sports including football and basketball.23,24 Therefore, there is not only evidence that all cartilage types in the skeletally immature are at risk for injury, but there is also a lack of understanding regarding maturation of tissue at the locality of knee OCD formation. These details, coupled with the comparative anatomy animal studies, suggest that the definition of OCD potentially could be adapted to read "a focal, idiopathic alteration of subchondral bone and/or its precursor with risk for disruption of adjacent articular cartilage that may result in premature osteoarthritis (Figure 2).”25
Figure 2. Schematic of a distal femur undergoing ossification in the epiphysis from left to right with an injury to the articular-epiphyseal cartilage complex that ultimately becomes an osteochondritis dissecans lesion as the surrounding and unaffected ossification front continues growth.
OCD formation related to the epiphyseal cartilage is not well studied in humans, although there is a single case report demonstrating sequential MRIs in two children first without and then with a clear OCD of the knee that suggests that a single traumatic event could result in an OCD lesion.26 For the patient in that report, there was no apparent involvement of their epiphyseal anlage cartilage on the initial MRI images, but they subsequently developed an OCD lesion. The purpose of this study was to determine if serial MRI imaging in children could identify the etiology of OCD development by localizing the area of pathology within the articular-epiphyseal cartilage complex. Understanding that OCD ultimately involves the articular cartilage (as an end point in the disease process), it is important to distinguish where the pathology starts (deeper to the articular surface due insufficient anatomic support). Given our understanding of cartilage types, the potential weak link in the articular-epiphyseal cartilage complex is the anlage cartilage of epiphyseal bone, which is what has been demonstrated in comparative anatomy studies.
Therefore, our hypothesis is that the anlage cartilage of epiphyseal bone is the site of injury in OCD in human children. Our primary aim was to compare the depth of the OCD relative to the physis both before and after OCD development in the same children (including measures of original trauma, if present) to determine the location of pathology. The secondary aim was to determine if the response to injury seen in comparative anatomy studies (the halting of ossification) was also seen in human cases of knee OCD.
Methods
A retrospective review was performed after obtaining Institutional Review Board approval (#170520X) utilizing two different institutional OCD databases. All children were under the age of 18 years old, and they were included for measurements if they had an antecedent Index-MRI of the same knee before their presentation for their distal femoral OCD. Demographics were recorded for each child, including the history of why each Index-MRI was obtained (since they were being seen prior to the development of an OCD lesion).
MRI images had been performed on either a 1.5T Signa Scanner (General Electric Healthcare, Milwaukee, WI) or a 1.5T Symphony System (Siemens Medical Solutions, Iselin, NJ). T1 fat saturation axial imaging, T1-weighted spin-echo pulse sequence coronal and sagittal imaging, and T2-weighted fat saturated sequence coronal and sagittal imaging were utilized for measuring the parameters of interest at 4 mm intervals. Measurements were made directly on digital software AMICAS PACS (AMICAS Inc., Brighton, MA) utilizing the supplied ruler tool. Measures were made on sagittal, coronal, and axial sequences to obtain width, height, and depth of the affected condyle on the Index-MRI and the OCD-MRI (their second MRI but first MRI obtained for their OCD workup) for measures of normal growth. The presence and height of marrow edema, the distance from the primary physis to the site of the future OCD lesion, and the height (or thickness) of the epiphyseal and articular cartilage combined at the site of the future OCD lesion were measured on the Index-MRI in the planes that demonstrated the lesion on the later OCD-MRI (Figure 3A, 3B). Axial measurements were made in a similar fashion to the sagittal and coronal images. The patency of the physis, presence of marrow edema, the presence of signal change in the epiphyseal cartilage, and any associated findings were noted on the Index-MRI. Similar measures were recorded for the subsequent OCD-MRI on all three planes, with the thickness of epiphyseal and articular cartilage being replaced by the height of the OCD itself (Figure 3C, 3D). Measurements were obtained on the slice with the largest appearance of the OCD and working backwards in time, the like slice for the index MRI when the OCD was not present. The various depths were obtained by utilization of the proximal side (or ossified metaphyseal side) or the main physis as a landmark to account for changes in physeal width over time (or closure of the physis). On the articular side, the measurements were anchored on the delineated transition from articular cartilage to subchondral anlage cartilage if no OCD present or at the proximal portion of the OCD when present. The duration of time between the two images was also recorded.
Figure 3. MRI measurements. (A and B) Sagittal T1 and Coronal T2 fat saturation images demonstrating Index-MRI measures. (C and D) similar sequence and cuts in the later OCD-MRI measures indicating changes seen from Index-MRI to OCD-MRI. Measures on axial sequences were performed using the same landmarks.
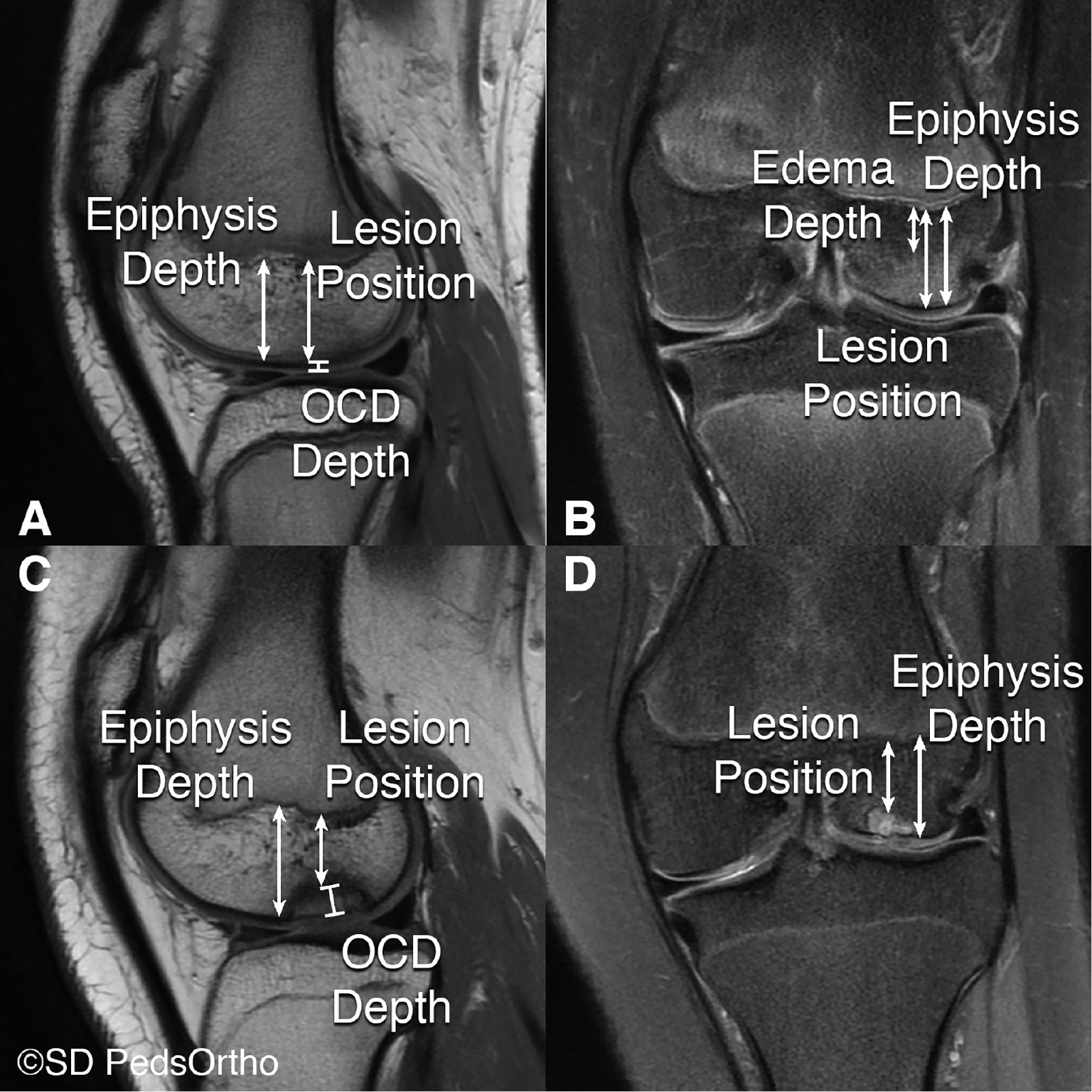
Measures between the two time points were then compared to determine if the height of the structures measured from OCD-MRI correlated with evidence of abnormality seen and measured on Index-MRI (Figure 4). A positive value of change in height, width, and depth measurements of the affected condyle adjacent to, but not including, the location of the OCD defined ‘Growth’. ‘Lesion Position’ was defined as the distance from the primary physis to the OCD itself, measured across the epiphysis, and a change in the lesion position over time was the difference between the two time points (a difference of zero mm suggesting that the injury at Index-MRI affected epiphyseal growth and ossification at that location). ‘OCD Depth’ was defined as the difference between the Index-MRI and OCD-MRI measurements of OCD height, with zero mm suggesting that the ossification front had not advanced around the OCD, a positive value that the surrounding normal ossification occurred, or a negative value that previously normal bone underwent necrosis adjacent to the injury (Figure 5).
Figure 4. A schematic drawing representing the possible changes seen in OCD depth and OCD position in the epiphysis from Index-MRI to the OCD-MRI.
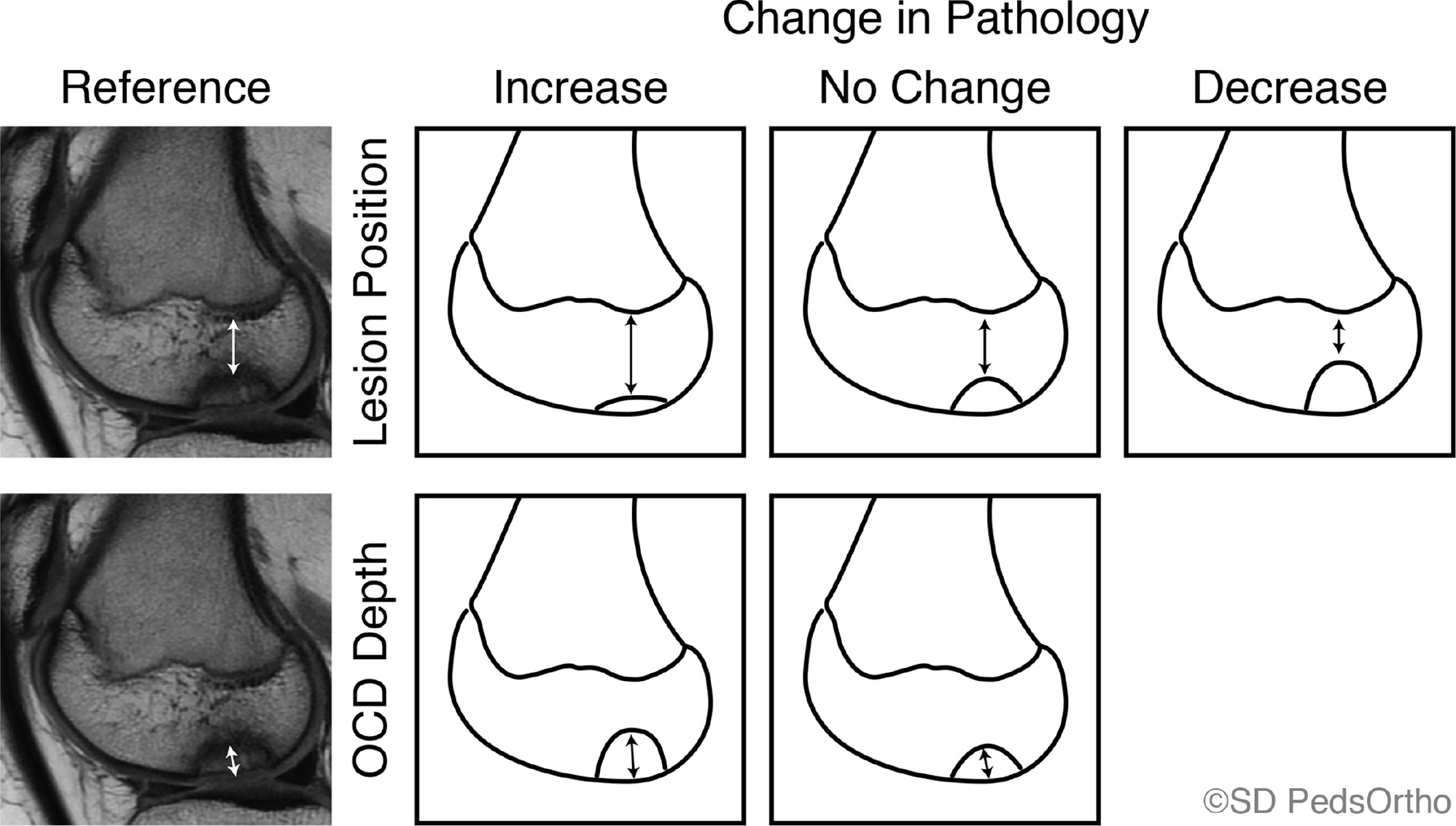
Figure 5. A flowchart that demonstrates the potential outcomes from the evidence of OCD development from Index-MRI to the OCD-MRI, highlighting at least three different responses to an injury at the articular-epiphyseal cartilage complex.
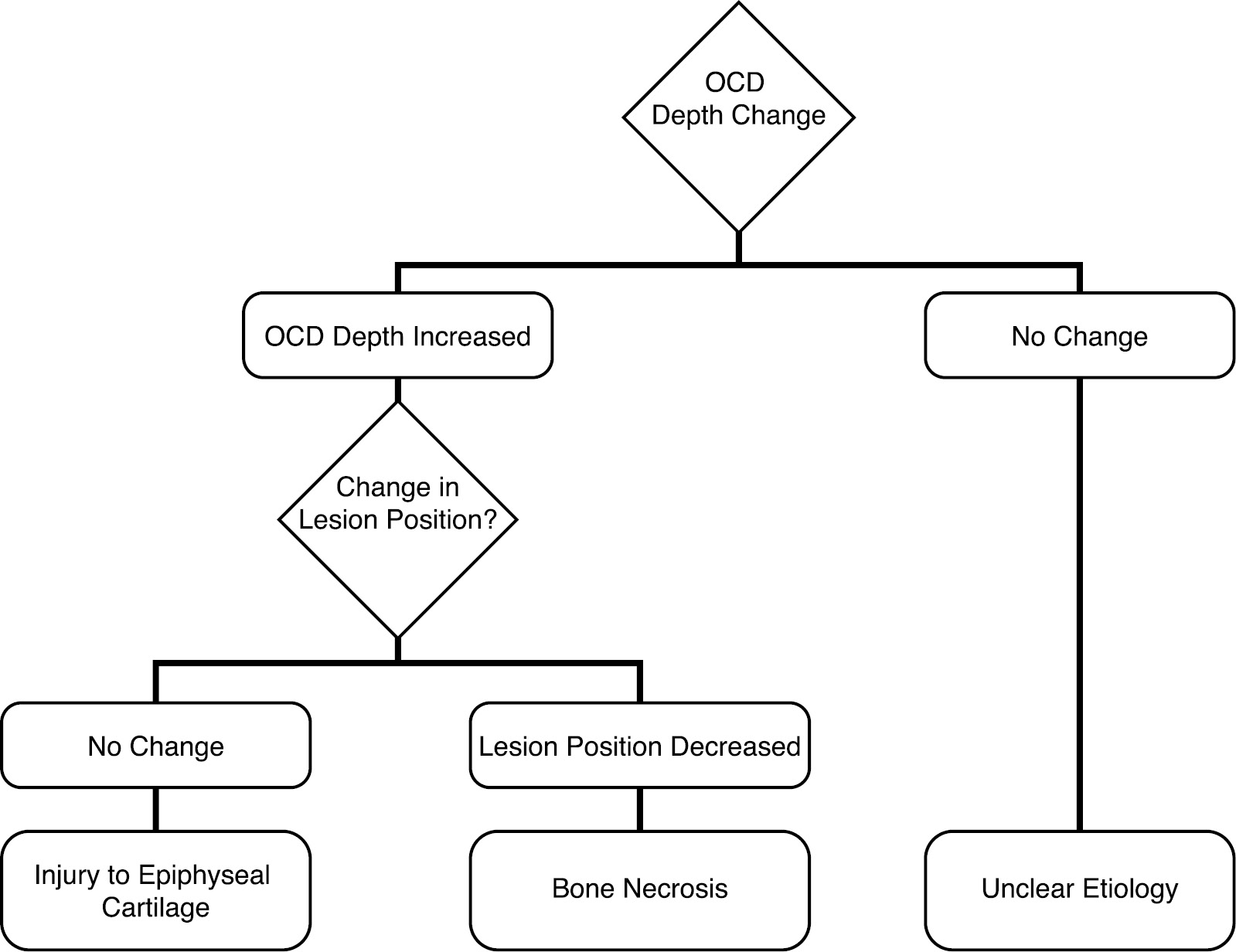
We determined three potential outcomes to the variables being measured. The first outcome is that an OCD lesion could increase thickness (positive change in ‘OCD Depth’) and not change position relative to the physis (a null change in ‘Lesion Position’) despite an overall ossifying growth of the epiphysis. This first scenario suggests that the OCD stemmed from an epiphyseal cartilage injury that halted the ossification front (the scenario suggested by comparative anatomy studies). By comparison, the second scenario is that there would be no change in OCD thickness despite overall epiphyseal ossifying growth (a null change in ‘OCD Depth’) and therefore an increased distance of the OCD from the physis (a positive change in ‘Lesion Position’). This second scenario is similar to the first in that it represents an injury to the epiphyseal cartilage epiphysis but contrasts in that it did not stall the adjacent ossification front. Finally, a third outcome is that the OCD thickness could increase (similar to the first scenario) but in the setting of a negative change in ‘Lesion Position’ (reduced size of the epiphyseal bone adjacent to the OCD) despite overall epiphyseal ossifying growth. This third scenario represents a “dieback” or avascular necrosis-type development within the epiphyseal bone itself.
Results
A total of 399 charts of children with knee OCD were screened for the presence of an antecedent Index-MRI, between two institutions over a period of 7 years. Six patients (seven knees) were available for radiographic assessment (two female/four male) all with open physes at the time of first MRI obtained at a mean 11.1 (median 11.6) years old (range 9.7 to 13.6 years). Index-MRI studies were obtained for a variety of reasons: both females had a patella instability event, two of the males had a history of traumatic presentation (one with 2 years of pain after lacrosse stick strike and swelling at the time and one was kicked in the knee during a soccer game), one male had no trauma (just “came home from school complaining”), and one obtained bilateral knee MRI for knee pain related to presumed enthesitis-related arthritis.
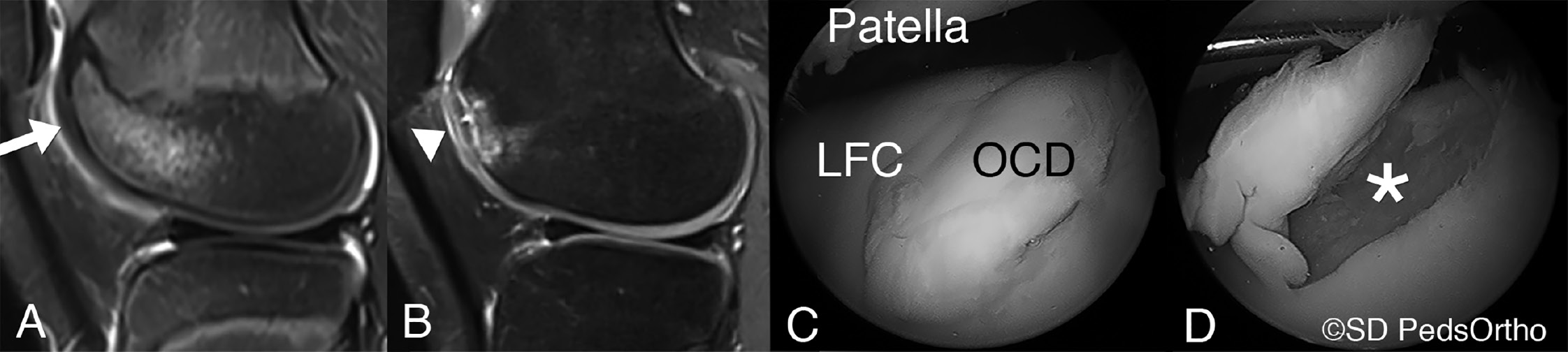
The mean time between Index-MRI and the OCD-MRI presentation was 2.4 (median 1.9) years (range 0.3 to 4.8 years), with a mean age of 13.5 (median 13.9) years old at OCD-MRI. At the time of OCD-MRI, two patients had closed their distal femoral physis and one was in the process of closing. One presented with a loose body associated with the OCD (Figure 6). Complaints at the time of OCD-MRI included: two patients with persistent pain (the two who had less than a 1-year duration between MRI, one without a traumatic event, and the other with a 2-year history of pain after a lacrosse injury), and the other four patients each presented with what they believed to be new onset knee pain not necessarily related to the previous complaint.
Figure 6. A case example: (A) Index-MRI of a 9-year-old girl who had a patella instability event (arrow indicating site of injury) with underlying bone marrow edema and was treated conservatively until (B) she returned at age 14.4 years with evidence of OCD on her OCD-MRI (arrowhead). Arthroscopic evaluation after the OCD-MRI demonstrated grade IV chondromalacia (C & D) with the asterisk indicating the subchondral bone.
Increased signal on T2 weighted images within the epiphyseal cartilage was noted on all but one of the patients on their Index-MRI, predominately involving the epiphyseal cartilage. However, the child with bilateral OCD development did demonstrate signal change within the epiphyseal cartilage on both knee Index-MRIs but not at the location where OCD ultimately developed. There were four cases that followed the described animal model pathology with what appears to be an injury to the epiphyseal cartilage (Figure 7). One case that appears to be more akin to osteonecrosis (Figure 8) and two cases that do not follow either of the previous two pathologic developments (Figure 9).
Figure 7. MRI images (sagittal and coronal T2 Proton Density with Fat Saturation) of children at initial presentation without OCD and at re-presentation with evidence of OCD in the knee. These examples demonstrate an injury to the epiphyseal anlage cartilage with subsequent normal growth around the lesion as described in the literature.
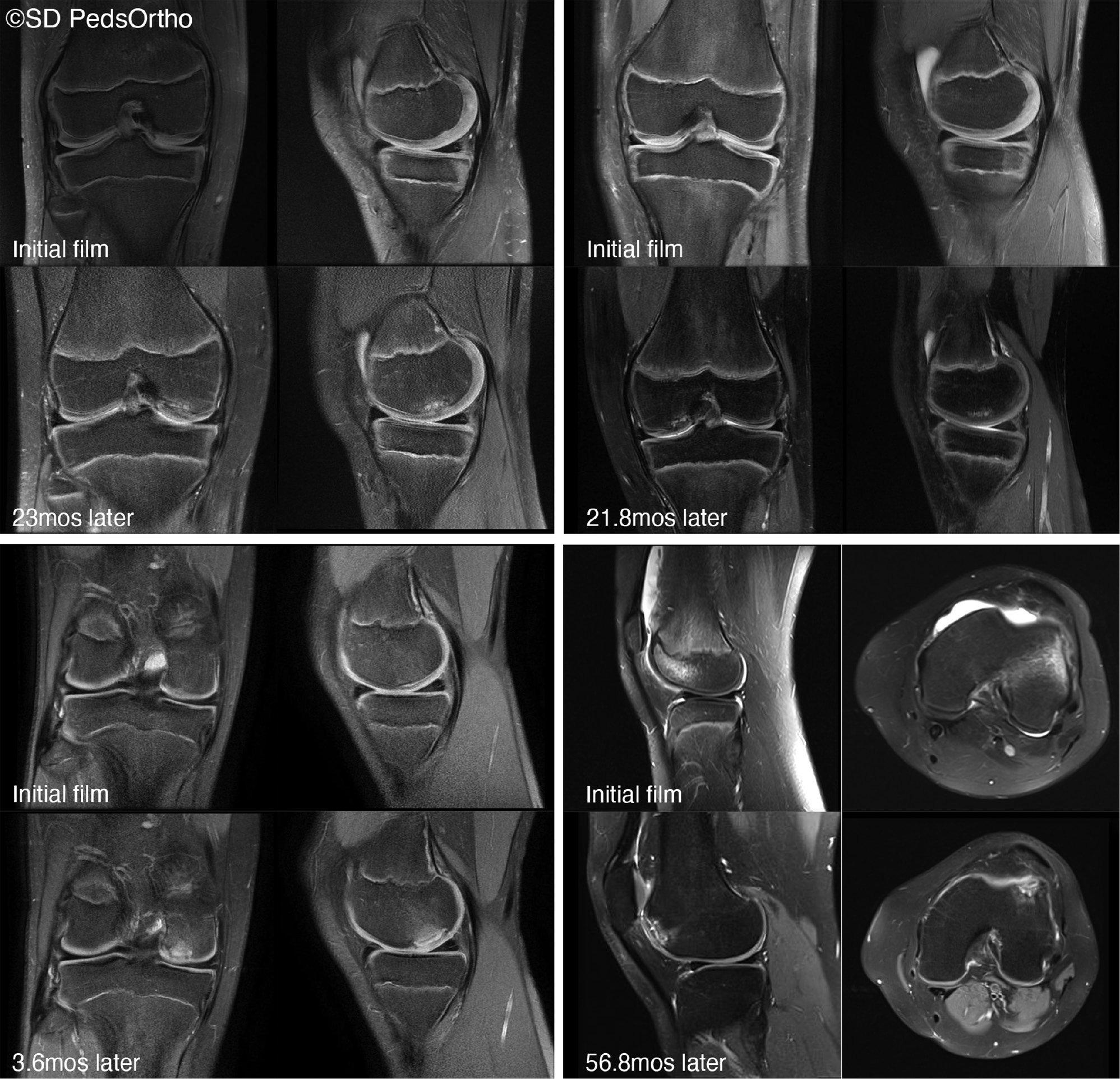
Figure 8. The single example of bone necrosis from initial to subsequent MRI imaging (sagittal and coronal T2 Proton Density with Fat Saturation).

Figure 9. The two examples of osteochondritis dissecans development from index to final MRI (sagittal and coronal T2 Proton Density with Fat Saturation) without a clear etiology identified in the flowchart from Figure 4.
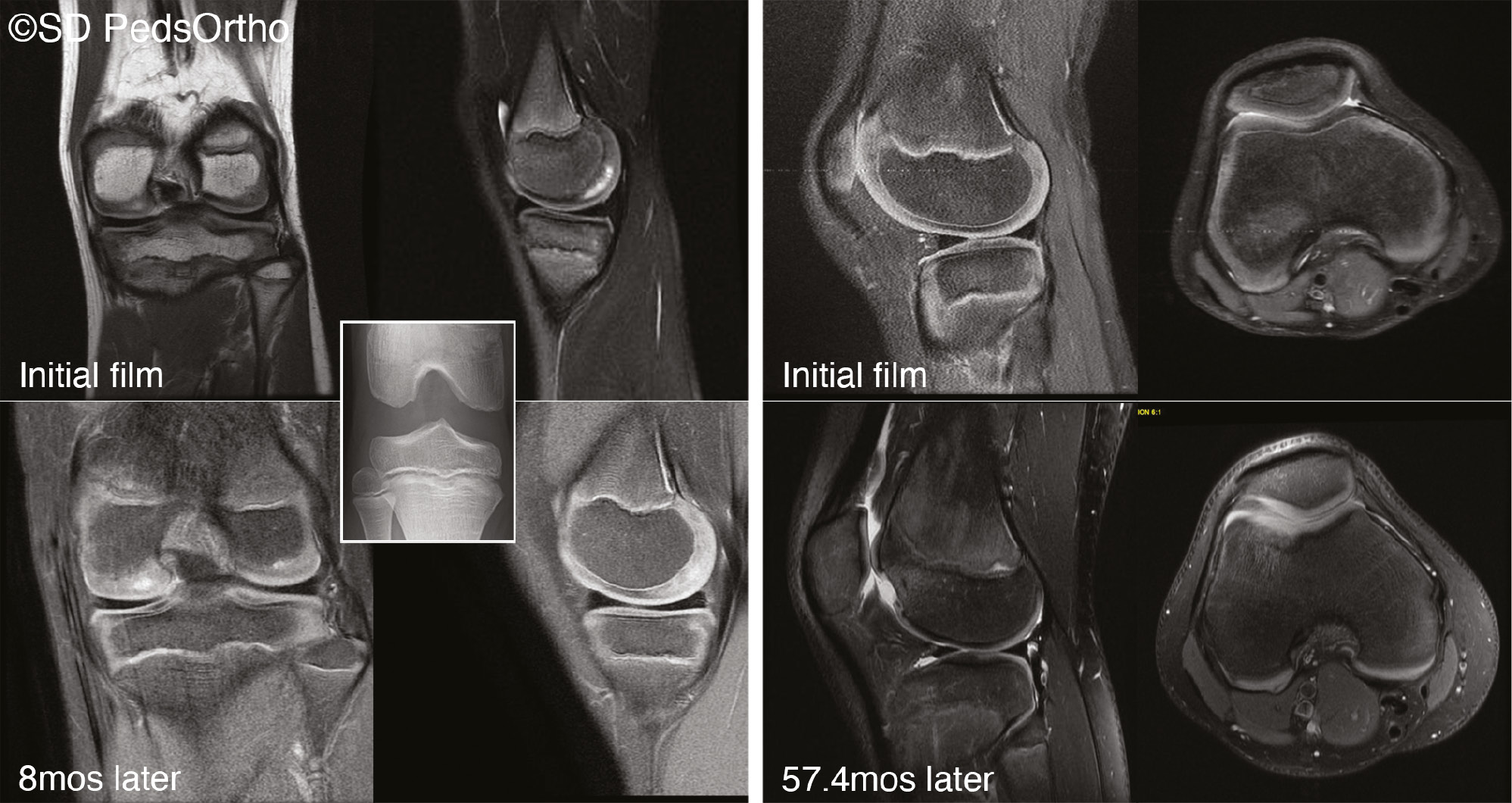
All the children demonstrated some ‘Growth’ over the interval between Index-MRI and OCD-MRI (Table 1). ‘Lesion Position’ did not shift significantly from zero (Table 2) as a group, but individually, there were two that went in a positive direction (growth of ossification front), four that did not demonstrate further ossification, and one that demonstrated epiphyseal bone necrosis with a negative value. ‘OCD Depth’ measures had mean positive values indicating that growth of the surrounding epiphyseal cartilage continued in the setting of stalled ossification at the site of OCD in both the coronal (p=0.029) and sagittal planes (p=0.026).
Table 1. Measurement Means and Medians at Both Time Points Within the Study
| n | Index-MRI |
OCD-MRI |
|||
|---|---|---|---|---|---|
| Mean ± SD | Median (Min-Max) | Mean ± SD | Median (Min-Max) | ||
| Age (years) | 7 | 11.1 ± 1.6 | 11.6 (9.2-13.6) | 13.5 ± 1.7 | 13.9 (9.9-15.0) |
| Coronal Epiphysis Depth | 7 | 24.3 ± 4.9 | 23.1 (17.8-33.9) | 26.8 ± 6.2 | 27.5 (19.1-34.7) |
| Coronal Lesion Position | 5 | 23.7 ± 3.3 | 24.4 (20.1-27.9) | 21 ± 5.0 | 21.2 (13.7-27.6) |
| Coronal OCD Depth | 5 | 4.2 ± 1.6 | 3.9 (2.1-6.1) | 7.2 ± 1.7 | 6.8 (5.6-9.7) |
| Depth of Marrow Edema (COR) | 5 | 7.7 ± 12.2 | 0 (0-27.9) | 14.9 ± 5.5 | 13.7 (8.3-20.8) |
| Sagittal Epiphysis Depth | 7 | 31.2 ± 11.9 | 24.4 (21.9-51.8) | 36.2 ± 16.4 | 28.3 (22.2-62.8) |
| Sagittal Lesion Position | 7 | 29.8 ± 12.8 | 23.3 (17.6-51.5) | 30.6 ± 15.2 | 23.3 (17.7-53.3) |
| Sagittal OCD Depth | 7 | 4.9 ± 2.4 | 4 (2.2-9.2) | 7.8 ± 1.6 | 8.5 (4.9-9.2) |
| Depth of Marrow Edema (SAG) | 4 | 21.5 ± 7.0 | 22 (13.7-28.4) | 20.4 ± 12.3 | 17.7 (8.5-46.0) |
| Axial Depth | 7 | 53.1 ± 6.9 | 55.1 (41.7-63.4) | 57.8 ± 4.2 | 57.7 (53.6-65.4) |
| Axial Lesion Position | 2 | 47.4 ± 8.0 | 47.4 (41.7-53.0) | 49 ± 0.4 | 49.0 (48.7-49.3) |
| Axial OCD Depth | 2 | 3.7 ± 1.7 | 3.7 (2.5-4.9) | 10.3 ± 0.3 | 10.3 (10.1-10.5) |
| Depth of Marrow Edema (AX) | 2 | 14.8 ± 20.9 | 14.8 (0.0-29.5) | 31.0 ± 20.9 | 31 (16.2-45.7) |
Table 2. Change in Time From Index-MRI to the OCD-MRI for the Primary Measurements in Millimeters
| n | Mean | Std. Deviation | Std. Error Mean | p-value | ||
|---|---|---|---|---|---|---|
| Growth | Coronal | 7 | 2.49 | 4.51 | 1.7 | 0.195 |
| Sagittal | 7 | 4.97 | 4.88 | 1.85 | 0.036a | |
| Axial | 7 | 4.67 | 5.03 | 1.9 | 0.049a | |
| Lesion Position | Coronal | 5 | -2.68 | 2.51 | 1.12 | 0.075 |
| Sagittal | 7 | 0.81 | 4.12 | 1.56 | 0.619 | |
| Axial | 2 | 1.65 | 7.57 | 5.35 | n/ab | |
| OCD Depth | Coronal | 5 | 2.98 | 2 | 0.89 | 0.029a |
| Sagittal | 7 | 2.96 | 2.66 | 1 | 0.026a | |
| Axial | 2 | 6.6 | 1.98 | 1.4 | n/ab |
abold value indicates p-value <0.05.
bindicates n=2, no p-value reported due to low sample size.
Discussion
The etiology of knee OCD remains elusive, even as we continue to develop improved models of understanding. The OCD lesions in our study appeared to form within the articular-epiphyseal cartilage complex, particularly at the anlage cartilage, and the injury appeared to most frequently stop the ossification front at the site of injury in a manner consistent with animal studies. However, since one patient in this limited series had apparent bone necrosis at the adjacent ossified epiphyseal bone, our results provide evidence that the etiology of knee OCD may not be a singular cause or that more than one injury pattern may result in the human OCD.
This is the first study to demonstrate growth of the epiphysis and cessation of the ossification front at the site of the OCD in humans, suggesting that growth of the OCD (increasing ‘OCD Depth’) is an increase in size (ossification) of the surrounding, unaffected bony epiphysis and not really a growth of the OCD lesion itself. However, we also demonstrated, in the single case, that previously normal ossified bone could undergo necrotic changes. Perhaps this variation means that knee OCD in humans does not form from a single etiology. The evidence in the literature,3–15 plus the Index-MRI and OCD-MRIs presented here, further indicate that OCD etiology does not, at least, result in a single pattern of disease whether a variation in the etiology or merely a variation in response.
During our assessment of this cohort of patients, we were expecting to see an injury to the anlage cartilage (osteochondritis occulta) and later the ossification front (osteochondritis manifesta), (as proposed by Laor and colleagues)24 or our first described scenario in the Methods (increased ‘OCD Depth’ and null change in ‘Lesion Position’), but we only identified this pattern in four of the seven knees. Although these individuals support our hypothesis towards OCD etiology being related to epiphyseal anlage cartilage injury, we need to consider the other three cases that differed from the expected pattern. Two children in our cohort still demonstrated some ossification between the OCD and the physis, our second possible scenario (an increased ‘OCD Depth’ and increased distance from the physis or ‘Lesion Position’). This injury pattern does not preclude an injury to the epiphyseal anlage cartilage; it only reduces the likelihood that the ossification front was damaged from the inciting insult. Finally, one patient clearly differed from this hypothesized epiphyseal anlage cartilage etiology. His OCD developed within the location of the previously ossified epiphysis (no evidence of anlage cartilage injury in the form of osteochondritis occulta), suggesting instead that avascular necrosis may be the etiology (our third scenario of reduced distance of the OCD to the physis or a decreased change in ‘Lesion Position’).
This “third scenario type” child who had a reduced distance from the physis to the OCD but with positive surrounding ossifying growth represents a “dieback” of avascular necrosis-type development. We did not see a correlation to the extent of bone marrow edema on Index-MRI and size of the OCD on subsequent imaging to suggest a correlation with extent of injury. It is important to understand that there is evidence in adults that this type of pathology exists. Spontaneous osteonecrosis of the knee, or SONK, is most commonly seen in patients who are 60 years of age or older.27 In addition, SONK is classically described as a focal, superficial subchondral lesion, mainly affecting the medial femoral condyle.28 This is supported by al-Rowaih et al., who demonstrated that in 109 patients who were diagnosed with SONK, the medial femoral condyle was affected 94% of the time (102 out of 109 knees).29 Furthermore, the medial femoral condyle predominance has been purported to be as a result of varying blood supply (watersheds) between the medial and lateral condyles. A cadaveric study by Reddy and Fredericks demonstrated that the medial femoral condyle has limited intra-osseous blood supply with apparent watershed areas, whereas the lateral femoral condyle has both a rich intra- and extra-osseous vascular supply.30 All of this sounds very similar to proposed etiologies for OCD in children; however, before we start thinking of OCD as being akin to SONK, it is important to understand that newer theories related to SONK suggest that osteonecrosis is a misnomer and that these older patients are actually sustaining fragility fractures; the unstable fracture is resulting in bone death of the displaced fracture fragment.28,31,32 The children in this study may not have sustained a fragility fracture, but they may have sustained subchondral fractures, and perhaps the etiology is similar.
The limitations of the study are inherent in the inability to have Index-MRI studies on all 399 patients in our study. This would take a prospective evaluation that may not be feasible in the modern era of medicine. Moreover, because of the retrospective design, we do not have all information about each child (activity level participation, flexibility scores, Beighton scores, etc.) that may be inherently important in fully understanding the etiology of OCD. Also, since children have the ability to heal or “regrow” from damaged tissue, we also cannot confirm or deny that the epiphyseal tissue may have grown into the traumatized tissue distally, creating a variable healing response that would impact our findings. Finally, the lack of contra-coup contusions on the tibia and the cases with very anterior trochlear contusions beg the question of how these injuries occurred, and how are they different than other bone contusions that do not evolve into OCD lesions?
This small cohort of children highlights that OCD development may have multiple patterns that ultimately lead to a similar final radiographic appearance and disruption of the articular cartilage. Most likely, the OCD begins with an injury to the articular-epiphyseal cartilage complex given the location of formation on the OCD-MRIs which supports our primary aim. However, we do not find unilateral support for our secondary aim, as development of OCD in these patients demonstrated different patterns: some completely stopped the ossification front of the epiphysis, others only slowed it down, and yet one appeared to develop a regression of ossification (likely bone necrosis) as the means to OCD development. Therefore, we would recommend that the definition of OCD be further adapted to read “a focal, idiopathic alteration in ossification of subchondral bone and/or the articular-epiphyseal cartilage complex with risk for instability and disruption of adjacent articular cartilage that may result in premature osteoarthritis.” With better understanding regarding the etiology of OCD, hopefully, we can better tailor future studies to hone in on the exact injury pattern to thereby improve our management of this focal end-stage disease in children.
Acknowledgements
The authors would like to thank Drs. Cathy Carlson, Jutta Ellermann, Alex Armstrong, and Ferenc Tóth at the University of Minnesota for supplying the SWI sequence for imaging, the vascularity of anlage cartilage, and feedback regarding the manuscript content. We also thank Kelly Boutelle for her assistance with manuscript preparation.
Disclaimer
No outside funding was received. The authors report no conflicts of interest related to this manuscript.
References
- Edmonds EW, Shea KG. Osteochondritis dissecans: editorial comment. Clin Orthop Relat Res. 2013;471(4):1105-1106.
- König F. The classic: on loose bodies in the joint. 1887. Clin Orthop Relat Res. 2013;471(4):1107-1115.
- Cahill BR. Osteochondritis dissecans of the knee: treatment of Juvenile and adult forms. J Am Acad Orthop Surg. 1995;3(4):237-247.
- Green WT, Banks HH. Osteochondritis dissecans in children. J Bone Joint Surg Am. 1953;35-A(1):26-47; passim.
- Bates JT, Jacobs JC, Shea KG, et al. Emerging genetic basis of osteochondritis dissecans. Clin Sports Med. 2014;33(2):199-220.
- Mubarak SJ, Carroll NC. Familial osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1979;(140):131-136.
- Mubarak SJ, Carroll NC. Juvenile osteochondritis dissecans of the knee: etiology. Clin Orthop Relat Res. 1981;(157):200-211.
- Yellin JL, Trocle A, Grant SFA, et al. Candidate Loci are revealed by an initial genome-wide Association Study of Juvenile Osteochondritis Dissecans. J Pediatr Orthop. 2017;37(1):e32-e36.
- Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg Br. 1971;53(3):440-447.
- Grimm NL, Weiss JM, Kessler JI, et al. Osteochondritis dissecans of the knee: pathoanatomy, epidemiology, and diagnosis. Clin Sports Med. 2014;33(2):181-188.
- Hefti F, Beguiristain J, Krauspe R, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8(4):231-245.
- Carlson CS, Meuten DJ, Richardson DC. Ischemic necrosis of cartilage in spontaneous and experimental lesions of osteochondrosis. J Orthop Res. 1991;9(3):317-329.
- Laverty S, Girard C. Pathogenesis of epiphyseal osteochondrosis. Vet J. 2013;197(1):3-12.
- Olstad K, Ekman S, Carlson CS. An update on the pathogenesis of osteochondrosis. Vet Pathol. 2015;52(5):785-802.
- Olstad K, Hendrickson EHS, Carlson CS, et al. Transection of vessels in epiphyseal cartilage canals leads to osteochondrosis and osteochondrosis dissecans in the femoro-patellar joint of foals; a potential model of juvenile osteochondritis dissecans. Osteoarthritis Cartilage. 2013;21(5):730-738.
- Rivas R, Shapiro F. Structural stages in the development of the long bones and epiphyses: a study in the New Zealand white rabbit. J Bone Joint Surg Am. 2002;84(1):85-100.
- Carlson CS, Hilley HD, Henrikson CK. Ultrastructure of normal epiphyseal cartilage of the articular-epiphyseal cartilage complex in growing swine. Am J Vet Res. 1985;46(2):306-313.
- Mackie E, Ahmed YA, Tatarczuch L, et al. Endochondral ossification: how cartilage is converted into bone in the developing skeleton. Int J Biochem Cell Biol. 2008;40(1):46-62.
- Chen G, Schuetz M, Pearcy M. Mechanobiology of bone development and computational simulations. In: Bronner F, Farach-Carson MC, Roach HI (Trudy), eds. Bone and Development. London: Springer; 2010:279-295.
- Lerner AL, Kuhn JL, Hollister SJ. Are regional variations in bone growth related to mechanical stress and strain parameters? J Biomech. 1998;31(4):327-335.
- Jaramillo D, Laor T, Zaleske DJ. Indirect trauma to the growth plate: results of MR imaging after epiphyseal and metaphyseal injury in rabbits. Radiology. 1993;187(1):171-178.
- Trueta J, Trias A. The vascular contribution to osteogenesis. IV. The effect of pressure upon the epiphysial cartilage of the rabbit. J Bone Joint Surg Br. 1961;43-B:800-813.
- Laor T, Wall EJ, Vu LP. Physeal widening in the knee due to stress injury in child athletes. AJR Am J Roentgenol. 2006;186(5):1260-1264.
- Laor T, Zbojniewicz AM, Eismann EA, et al. Juvenile osteochondritis dissecans: is it a growth disturbance of the secondary physis of the epiphysis? AJR Am J Roentgenol. 2012;199(5):1121-1128.
- Nissen CW, Albright JC, Anderson CN, et al. Descriptive epidemiology from the Research in Osteochondritis Dissecans of the Knee (ROCK) prospective cohort. Am J Sports Med. 2022;50(1):118-127.
- Shea KG, Jacobs JC, Grimm NL, et al. Osteochondritis dissecans development after bone contusion of the knee in the skeletally immature: a case series. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):403-407.
- Mears SC, McCarthy EF, Jones LC, et al. Characterization and pathological characteristics of spontaneous osteonecrosis of the knee. Iowa Orthop J. 2009;29:38-42.
- Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg Am. 2000;82(6):858-866.
- al-Rowaih A, Björkengren A, Egund N, et al. Size of osteonecrosis of the knee. Clin Orthop Relat Res. 1993;(287):68-75.
- Reddy AS, Frederick RW. Evaluation of the intraosseous and extraosseous blood supply to the distal femoral condyles. Am J Sports Med. 1998;26(3):415-419.
- Akamatsu Y, Mitsugi N, Hayashi T, et al. Low bone mineral density is associated with the onset of spontaneous osteonecrosis of the knee. Acta Orthop. 2012;83(3):249-255.
- Mont MA, Marker DR, Zywiel MG, et al. Osteonecrosis of the knee and related conditions. J Am Acad Orthop Surg. 2011;19(8):482-494.