Current Concept Review
Pediatric and Adolescent Medial Collateral Ligament Injuries
1Children’s Hospital of the King’s Daughters, Norfolk, VA; 2Central Texas Pediatric Orthopedics, Bryan, TX; 3Vanderbilt University Medical Center, Monroe Carell Jr. Children’s Hospital, Nashville, TN; 4Walter Reed National Military Medical Center, Bethesda, MD; 5Children’s Hospital Orange County, Orange, CA; 6Rady Children’s Hospital, San Diego, CA; 7Children’s Hospital Colorado, Denver, CO; 8Children’s Hospital of Atlanta, Atlanta, GA; 9The Children’s Mercy Hospital, Kansas City, MO; 10Central Texas Pediatric Orthopedics, Austin, TX
Correspondence: Stephanie S. Pearce, MD, Nemours Children’s Health, 807 Children’s Way, Jacksonville, FL 32207. E-mail: [email protected]
Received: July 1, 2023; Accepted: September 18, 2023; Published: November 15, 2023
Volume 5, Number 4, November 2023
Abstract
Frequently overlooked, medial collateral ligament (MCL) injuries constitute a high percentage of sports-related injuries in pediatric and adolescent patients, and a nuanced approach is required to optimize outcomes in this unique patient population. We present a current concept review on MCL injuries to better define anatomic, clinical, and treatment applications unique to the pediatric and adolescent patient. Injury assessment in this age group must include a comprehensive knee exam evaluating for associated injuries unique to developing patients. Imaging can include a four-view knee series, stress radiographs, and alignment films to guide and follow treatment. To optimize patient outcomes, a detailed understanding of patient-specific factors related to knee anatomy and biomechanics during development are essential, along with appropriate characterization and classification of injury severity. The majority of MCL injuries in this age group can be managed nonsurgically with a thoughtful approach to rehabilitation, based on clinical and radiographic assessment. Some injuries may benefit from surgical intervention, such as primary repair versus reconstruction. The goal of this is to restore normal mechanics without compromising growth and development.
Key Concepts
- The superficial MCL is the main stabilizer of the medial aspect of the knee from valgus load and helps protect the Anterior Cruciate Ligament (ACL) from rupture or re-tear.
- Nonoperative treatment with bracing, activity modifications, and a formal physical therapy program is the first line of treatment for skeletally immature patients.
- Valgus stress radiographs are the preferred method of diagnosing an MCL tear that may be resistant to nonoperative intervention and require operative treatment.
- Operative treatment with reconstruction is recommended over repair for persistent medial instability or gapping >3mm seen on stress radiographs after 4-6 weeks of nonoperative treatment.
- Reconstruction is currently recommended with all epiphyseal femoral tunnel and physeal spanning tibial reconstruction to recreate the anatomic landmarks of the superficial MCL.
Introduction
Historically, studies looking at MCL injuries in pediatric patients have focused on combined ligament injuries associated with anterior cruciate ligament (ACL) tears.1 Isolated MCL injuries have been overlooked, but recent studies have reported on the anatomy and imaging aspects of isolated MCL injuries in pediatric patients.2–4 Traditionally, MCL injuries in pediatric patients have been treated nonoperatively, but surgery for MCL injuries is starting to be recommended.5 Whether treated nonoperatively or with surgery, physical therapy rehabilitation is important after a patient sustains an MCL injury. This current concept review of pediatric and adolescent MCL injuries covers intake to treatment with physical therapy protocols and expected outcomes.
Epidemiology of Pediatric MCL Tears
MCL injuries in pediatric populations have become increasingly common. Age does play a factor in the incidence, with children less than 10 years of age making up only 0.04% of cases in a large Swiss epidemiologic study.6 Soccer and skiing were responsible for 61% of these MCL injuries.6 Rate of 0.33 per 10,000 athletic exposures was found in a large cohort study in high school girls lacrosse.7 Kramer et al. looked at both isolated MCL and lateral collateral ligament (LCL) injuries and found that 66% of injuries occurred in contact sports with 28% of patients who sustained an MCL tear having a concomitant patellar instability event.2 They also found football injuries were more commonly grade III tears, and all grade III injuries occurred in either football or soccer.2 Data from the national high school sports-related injury surveillance study showed that MCL injuries accounted for 32.9% of all sports-related injuries in male athletes and 12.5% in female athletes.8
Anatomy and Biomechanics of the Medial Collateral Ligament
The medial knee consists of several interconnected structures that contribute to the overall stability of the knee joint. The MCL complex consists of three portions: (1) the superficial medial collateral ligament (sMCL; alternatively termed the tibial collateral ligament) (2) the deep medial collateral ligament (dMCL; alternatively termed the mid-third medial capsule ligament), and (3) the posterior oblique ligament (POL).9 Understanding the anatomy as well as the biomechanics of each of these structures is essential for evaluating and appropriately treating medial knee injuries.
Superficial MCL
The sMCL is the primary static restraint to valgus stress but also stabilizes internal and external rotation.9–12 Shea et al. evaluated pediatric cadaver specimens and found the MCL insertion is distal to the femoral physis with a median distance of 12 mm in the youngest group and decreases to 8 mm in the older group.12 The tibial insertion was well distal to the proximal tibia physis at 3 cm in the youngest group and 4.8 cm in the older group.13 Schmidt et al. tested the mechanical properties of pediatric knee collateral ligaments and found the overall stress and strain properties were weaker than what has been described in the adult literature.11,14
Deep MCL
The dMCL is a thickening of the joint capsule that attaches the medial meniscus to the femur and tibia through the meniscofemoral and meniscotibial ligaments.9 The meniscotibial ligament is shorter and thicker than the meniscofemoral ligament with an attachment 3.2 mm distal to the joint line.9 The meniscofemoral ligament inserts 15.7 mm proximal to the femoral joint line.9 The dMCL acts as a secondary stabilizer against valgus stress of the knee at all degrees of knee flexion and has a much lower valgus load to failure (101N) compared to the sMCL.11
Posterior Oblique Ligament (POL)
The POL is an expansion of the posteromedial knee capsule that arises from the distal aspect of the semimembranosus tendon and consists of superficial, central, and capsular arms.9 The central arm is the most important in terms of biomechanics and reconstruction techniques. The POL is the primary restraint of internal rotation.10 The POL also functions to complement the superficial MCL to resist valgus in early flexion as well as anterior and posterior tibial translation.12 The central arm of the POL attaches to the femur 1.4 mm distal and 2.9 mm anterior to the gastrocnemius tubercle.9 The POL has a valgus load to failure of 256N, placing it between what is seen with the superficial and deep MCL.11
Clinical Diagnosis
Patient Evaluation
The importance of a comprehensive history, especially recording the mechanism of injury, onset, and length of symptoms, as well as a thorough knee physical examination cannot be overemphasized.
During the history, pay attention to pain not related to activity (e.g., night pain, pain at rest) and a clinical course that does not follow a normal course of recovery.15 In a pediatric patient, the physical examination should always include an assessment of gait (when possible), hip range of motion (to rule out a slipped capital femoral epiphysis), standing alignment, secondary sexual characteristics (to assess skeletal maturity and residual growth). Examination is compared to the uninjured contralateral knee. When a clinician suspects an MCL injury, the following findings and examination maneuvers are of particular importance.
- Inspection
Thigh atrophy can be a sign of a chronic problem and cannot be attributed to a recent traumatic etiology. Epiphyseal lesions of the growing knee may masquerade as a proximal MCL injury in an active child. Standing coronal plane alignment is assessed for varus or valgus malalignment. Specifically look for any unilateral excessive valgus alignment of the affected extremity, as this may be a result of hemiphyseal arrest of the lateral distal femur from excessive stresses across the physis, which can be seen in youth kickers.16 Gait examination is performed specifically assessing for any dynamic knee valgus with gait. The presence of an effusion, when observed, should alert the clinician to have a high index of suspicion for other intra-articular pathology. - Presence and location of medial soft tissue swelling and/or ecchymosis
Depending on the acuity of the injury, this may vary. - Location of tenderness
Most commonly, the MCL injury occurs proximally near the medial epicondyle, but tenderness may be elicited along the mid-substance of the ligament or along the distal insertion of the superficial MCL near the pes anserine (6-7 cm below the joint line). While the medial joint line should be palpated for tenderness, the lateral joint line should also be scrutinized since the valgus mechanism responsible for MCL injuries also created a compressive load of the lateral compartment that may result in a lateral meniscus tear or a lateral side bone injury. - Valgus stress test
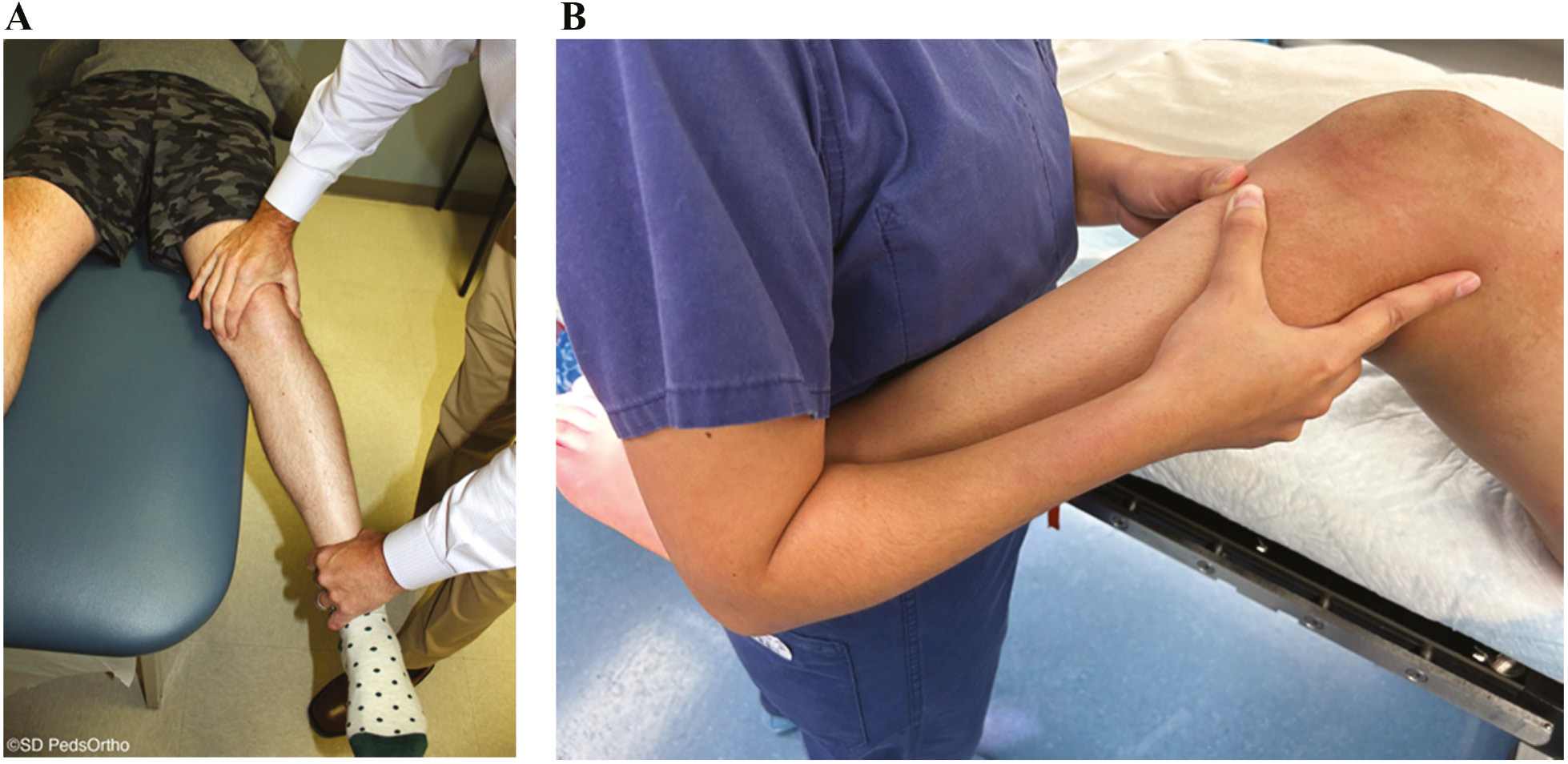
This maneuver is the single most important examination when assessing a patient with a possible MCL injury. This test should be performed in full extension as well as with the knee flexed 15-30 degrees. Laxity in full extension represents a high-grade MCL injury involving the entire MCL (superficial and deep fibers) as well as the posteromedial secondary stabilizers or the cruciate ligaments. Isolated laxity in flexion represents a lower-grade injury that is less likely to require surgical intervention. A reproducible technique for assessing medial-sided instability includes flexing the knee over the examination table. The thumb and middle or index finger of the examiner’s hand can then palpate and quantify any gapping of the joint while the examiner’s other hand applies a valgus force to the extremity. In children where body habitus may be a challenge, placing the distal aspect of the affected extremity into the examiner’s axilla while palpating the joint lines and applying valgus stress at 0 and 30 degrees of knee flexion may ease the experience for both the child and practitioner (Figure 1A and B).
Figure 1. (A) Valgus stress test performed with the patient’s knee flexed 15-30 degrees over the examination table with the examiner’s fingers palpating any gapping at the medial joint line. (B) Alternative technique that can be utilized in a patient with a larger leg.
An MCL injury is frequently associated with an ACL tear or a patella dislocation, so these knees should be examined with this in mind.
Classification
While multiple classification schemes have been developed for MCL injuries, all of them have limitations and none have been validated in the pediatric patient population. However, Fetto and Marshall developed a classification that may be applicable to the pediatric population17 (Table 1).
Table 1. Fetto and Marshall MCL Classification Scheme17
| Grade | Description |
|---|---|
| I | No presence of valgus laxity in 0 or 30 degrees of flexion |
| II | Stable in 0 degrees of flexion, valgus laxity in 30 degrees of flexion |
| III | Valgus laxity in both 0 and 30 degrees of flexion |
Imaging
Radiographs
At a minimum, two radiographs (AP/lateral views) of the knee should be obtained, but a four-view series (AP/lateral/merchant/tunnel views) may be preferable to minimize the chance of missing other pathology. Examples would be a Salter-Harris III fracture of the medial femoral condyle, which represents a transitional fracture that is seen in adolescents near skeletal maturity as an alternative to an adult MCL injury (Figure 2). Additional injuries to the MCL complex include medial epicondyle fractures or fractures to the most prominent aspect of the medial condyle, bony avulsions of the deep MCL, which are frequently associated with ACL tears (Figure 3), or even the rare Salter-Harris I or II fracture of the proximal tibia in which the MCL can become interposed within the fracture (Figure 4). With longer-term follow-up, periosteal avulsions of the MCL adjacent to the medial epicondyle may result in the formation of a Pellegrini-Stieda lesion where ossification of the proximal MCL is present from either a previous avulsion of the MCL or ossification within the MCL from a chronic tear/injury pattern (Figure 5). In cases of chronic instability with suspected genu valgum, a long leg alignment film is helpful in quantifying any underlying coronal plane malalignment that may need to be corrected simultaneously or prior to a ligamentous reconstruction.
Figure 2. 15-year-old male football player with a Salter-Harris III fracture of the medial femoral condyle (pink arrows).
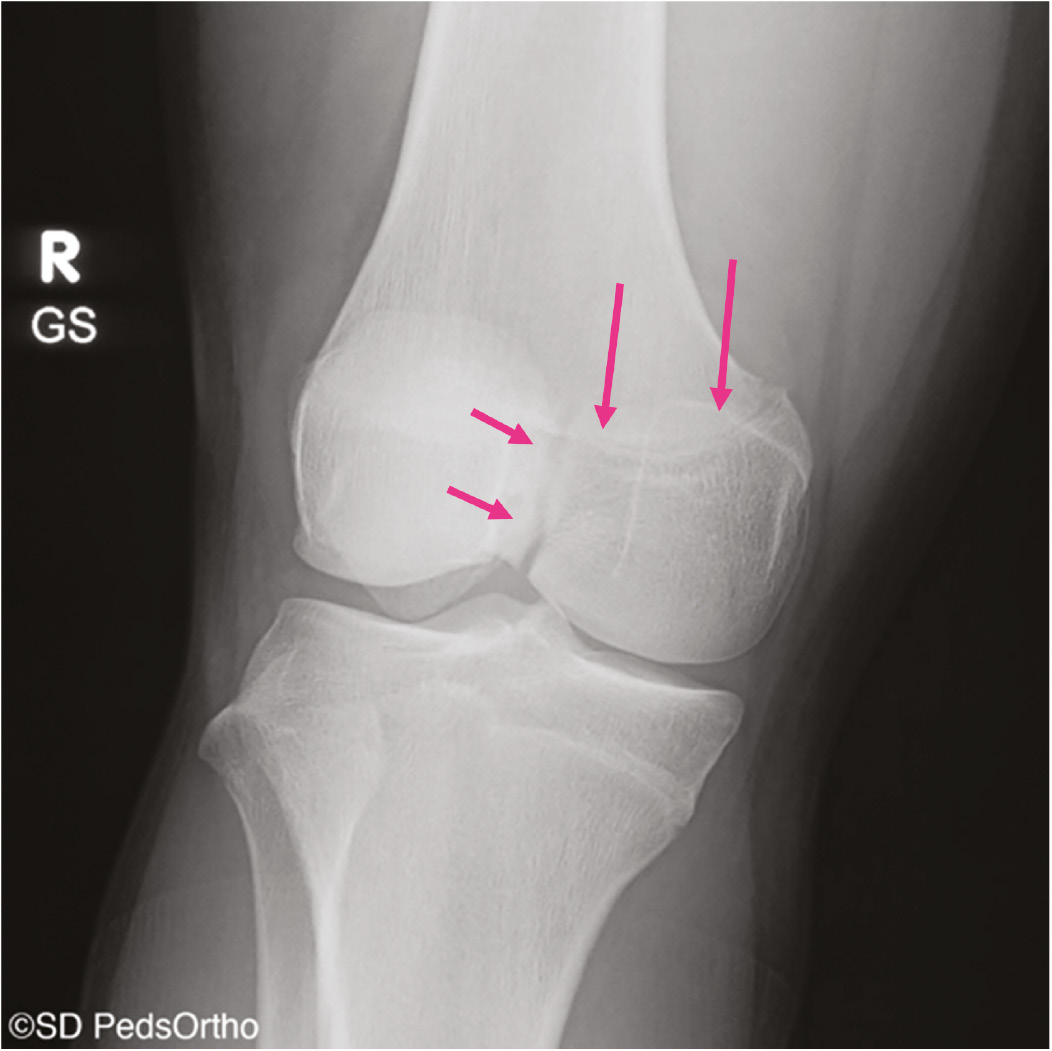
Figure 3. (A) AP radiograph demonstrating a bony avulsion of the proximal deep MCL (orange arrow). (B) Coronal image better demonstrates the deep MCL avulsion (blue arrow).
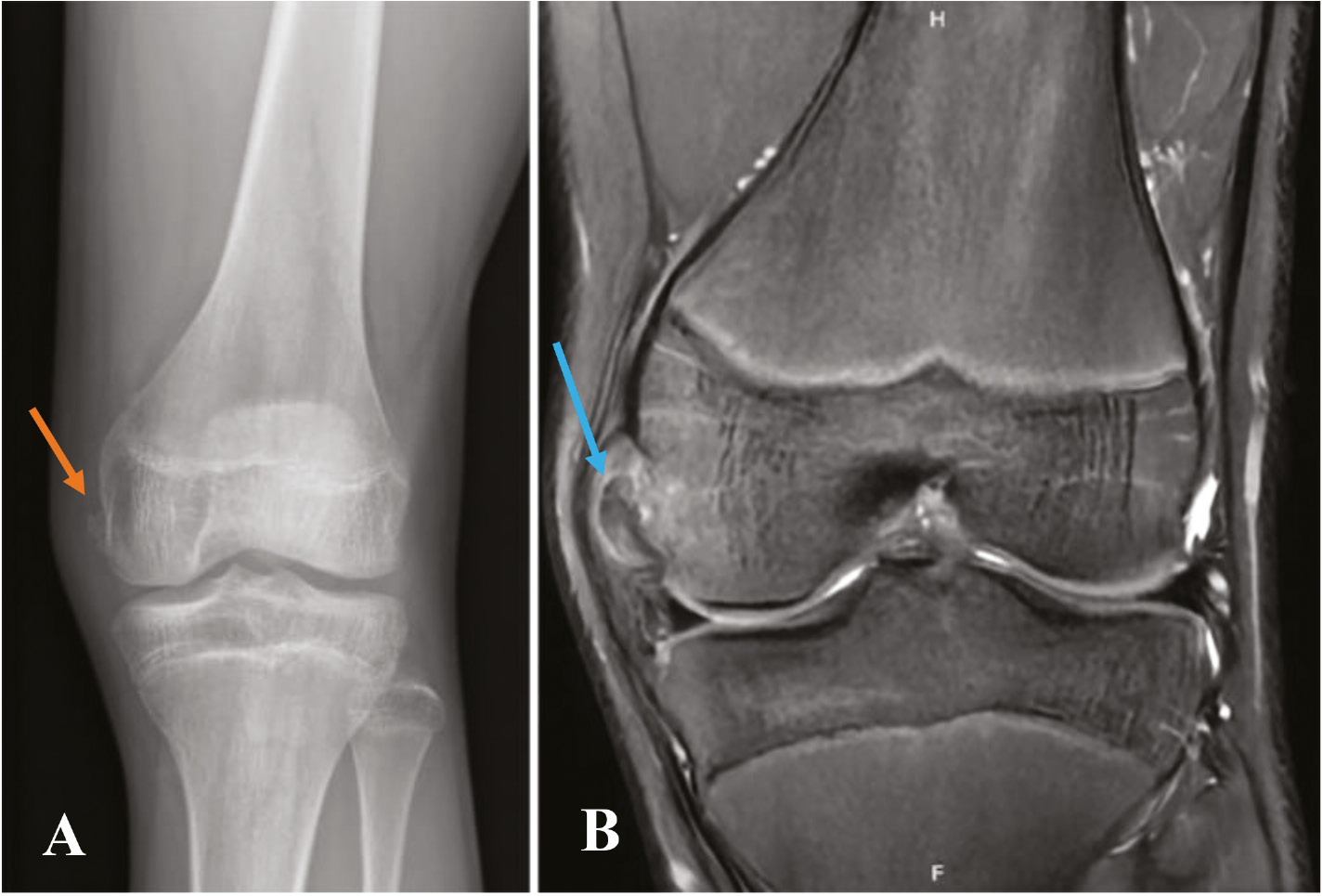
Figure 4. 12-year-old male with a left knee injury with a Salter-Harris I fracture of the proximal tibia with (A) asymmetric widening of the medial physis (green arrow) with (B) a coronal MRI image demonstrating the distal fibers of the superficial MCL interposed within the fracture (pink arrows).
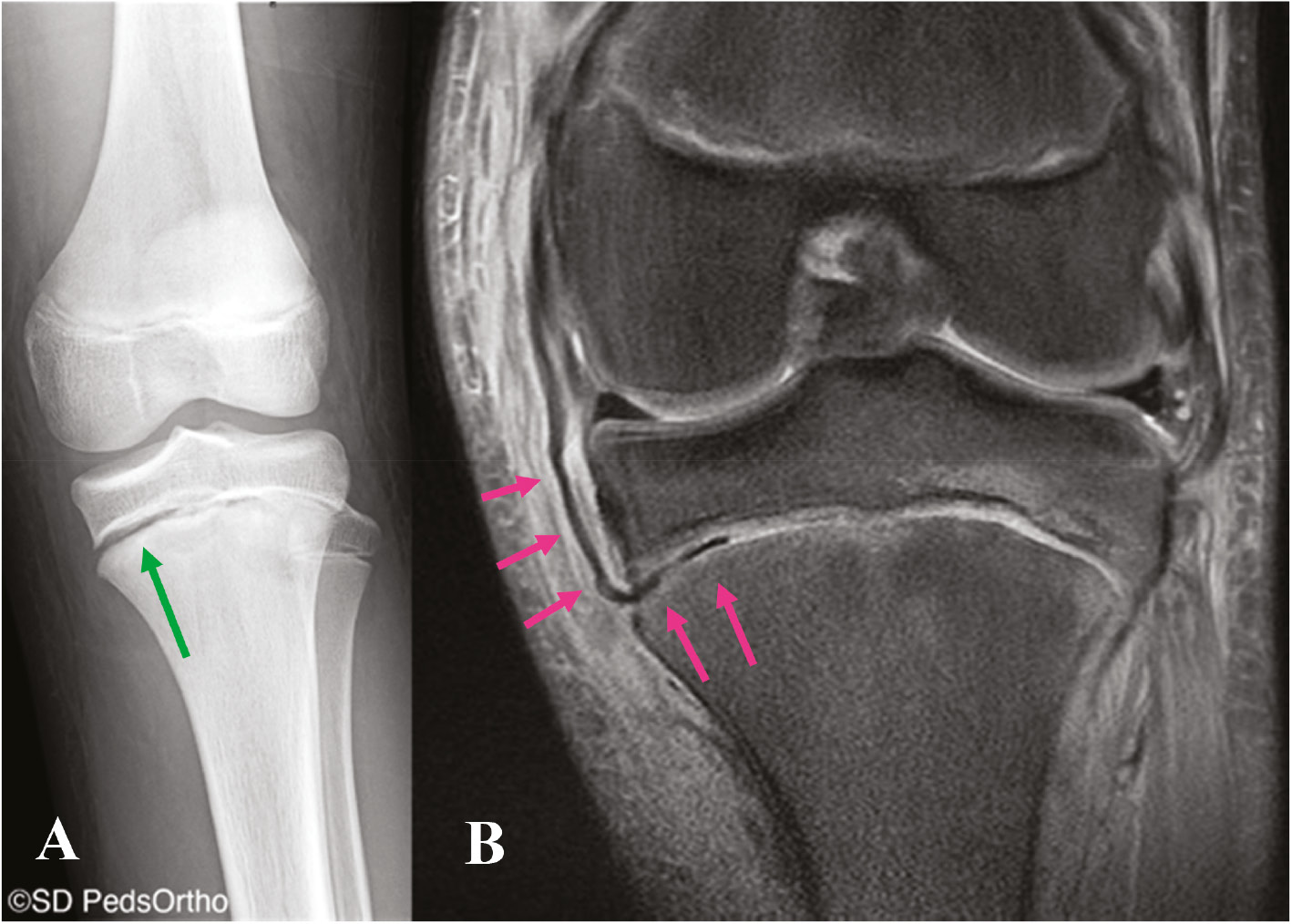
Figure 5. AP radiograph showing a Pellegrini-Stieda lesion (orange arrows) with ossification within the proximal MCL suggesting a chronic tear/injury pattern.

Stress Radiographs
Stress radiographs have become increasingly important in the workup and management of medial-sided knee injuries. These radiographs help objectively assess the extent of the medial-sided injury. While established thresholds exist in the adult population, these have not been validated in pediatric patients. Stress radiographs are performed with the practitioner applying a valgus stress to the extremity with the patella pointed towards the ceiling and the knee flexed 15-30 degrees (Figure 6). The uninjured contralateral extremity is also imaged and serves as a comparison. It is usually more successful to begin imaging the uninjured extremity to decrease anxiety associated with obtaining these stress images on the injured leg. Additionally, timing the stress maneuver with the radiographer minimizes the amount of time stress is held. Most patients tolerate these stress views without significant discomfort. The gapping between the medial femoral condyle and the medial tibial plateau is measured and compared to the uninjured extremity (Figure 7).
Figure 6. Technique for performing valgus stress radiographs.

Figure 7. Valgus stress radiographs of a patient with a complete tear of the superficial MCL seen with a 3 mm side-to-side difference between the left and right knees.

CT Imaging
CT scans aren’t routinely necessary for MCL tears but may be considered to evaluate the osseous architecture, a bony avulsion of the MCL, or in cases where a physeal injury is suspected (Figure 8).
Figure 8. Coronal CT image of a Salter-Harris III fracture of the medial femoral condyle in an adolescent patient presenting with a mechanism and examination concerning a proximal MCL injury.

Magnetic Resonance Imaging
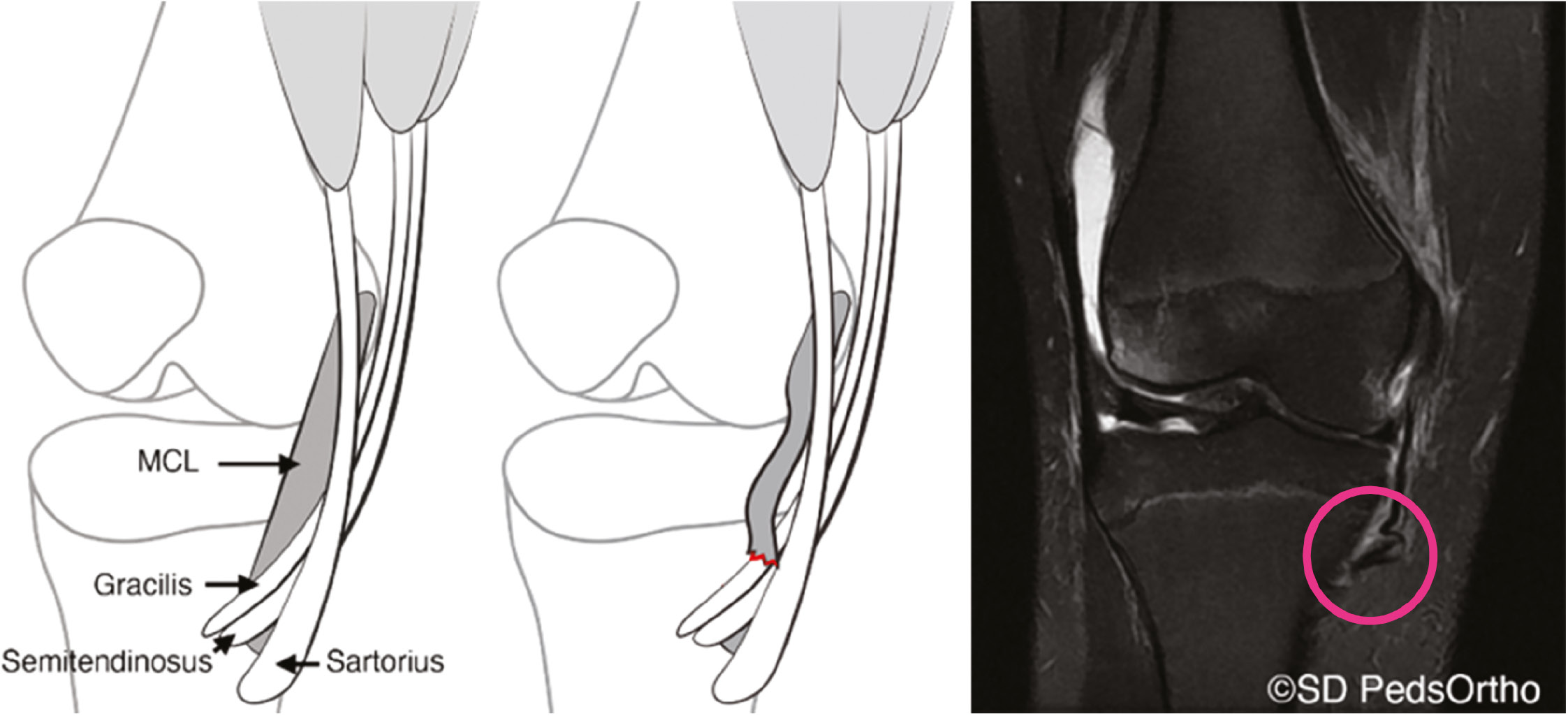
In cases where significant medial instability is encountered on exam or with stress radiographs, an MRI is indicated to assess the extent of the medial-sided injury as well as to evaluate the bone, menisci, cartilage, and surrounding ligamentous structures. Furthermore, if an effusion is encountered on examination, an MRI is indicated to better assess a concomitant intra-articular injury. Once obtained, the medial structures should be individually scrutinized including the dMCL, the sMCL, and the underlying meniscus. This will give a better sense of the extent of the injury as well as the healing potential (Figure 9). Distal ruptures of the superficial MCL injury with the ligament flipped over the pes tendons (Stener-like lesion) likely have the worst healing potential and may require surgical intervention (Figure 10).18
Figure 9. Coronal images of two different patients with proximal MCL injuries of differing severities. Figure 9A demonstrates a complete tear of both the deep (blue arrow) and superficial (orange arrow) fibers of the proximal MCL injury, whereas Figure 9B demonstrates a partial tear of the proximal MCL (pink arrows).
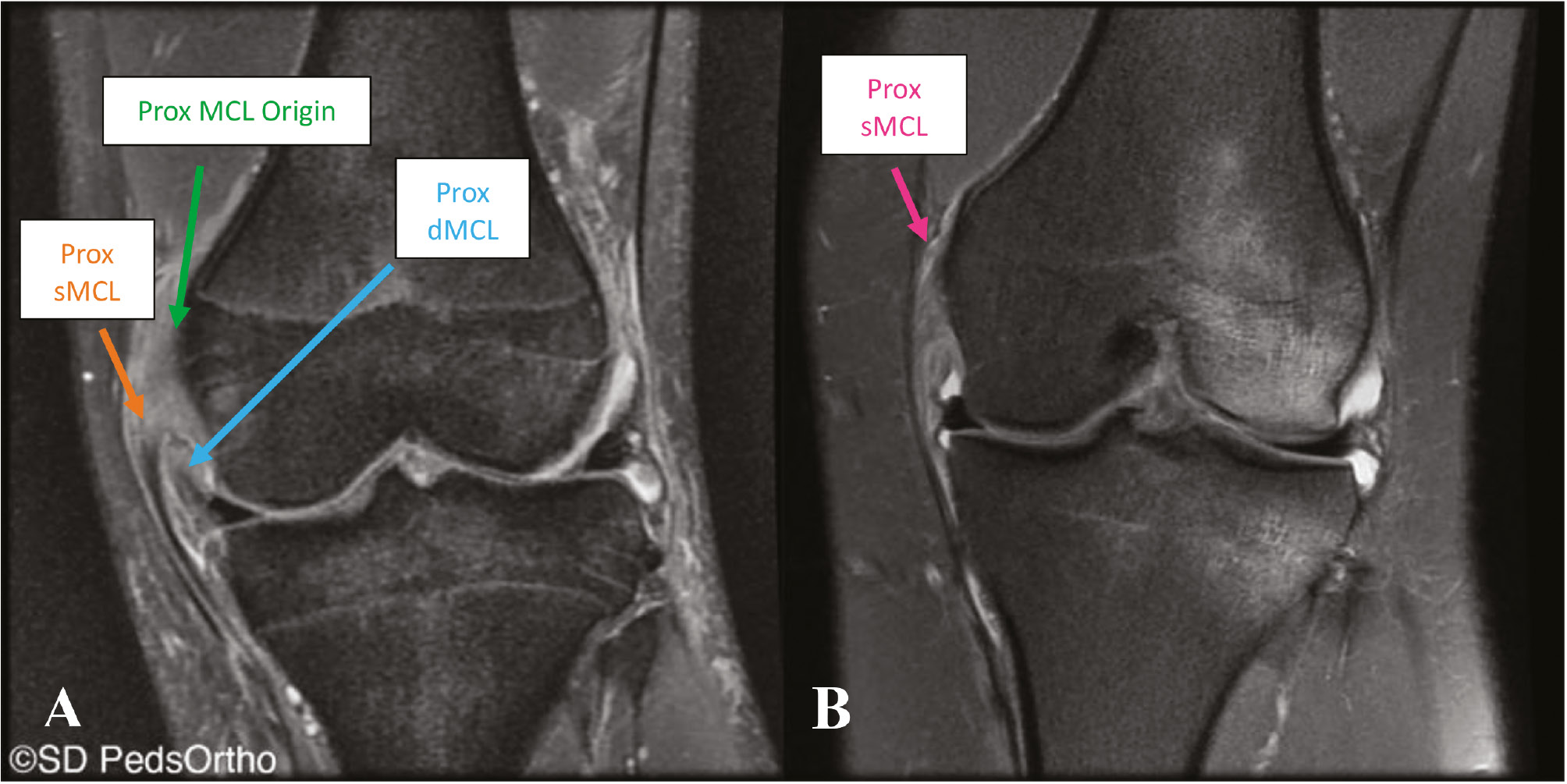
Figure 10. Stener-like lesion (pink circle) of the distal MCL with the superficial MCL avulsed from the tibia and flipped over the pes tendons.
Treatment: Nonoperative
Prior to initiating nonoperative management, care must be taken to ensure that the knee is not in valgus alignment and that there are no other ligamentous injuries on physical exam.19,20 As described above, MRI can be helpful in identifying concomitant injuries as well as the location of the injury, as these factors play a significant role when considering treatment options.
The healing response of the MCL occurs in four distinct phases of hemorrhage, inflammation, repair, and remodeling.21 The resultant scar tissue has been found to have a disorganized matrix, decreased collagen crosslinking, and hypercellular areas. This has been hypothesized to explain the biomechanical inferiority of post-injury MCL tissue when compared with native tissue.22 While this has not been fully elucidated clinically, it may explain long-term laxity seen in the nonoperative management of MCL injuries.23
The role of bracing and immobilization in the treatment of MCL injuries has been extensively studied. Prolonged immobilization after MCL injury has a deleterious effect, and clinical studies support early range of motion stabilized by a brace.24,25 Bracing consists of either medial and lateral or lateral-only hinged support, which is initiated as soon as the patient can tolerate motion in the knee and continues for 3-6 weeks.
Other nonoperative treatment modalities such as ultrasound, laser, hyperbaric oxygen, and direct current in the treatment of MCL injuries have shown promise in animal studies, especially in regard to early healing.26–28 Future clinical trials are needed to better determine the role of these modalities in the nonoperative management of MCL injuries.
Physical Therapy for Nonoperatively Treated MCL Injuries
Injuries to the MCL that do not require surgery will benefit from skilled rehabilitation to ensure the protection of healing tissues, full recovery of function, and safe return to pre-injury level of activity for the pediatric patient.
The initial goal of rehabilitation for nonoperative MCL injuries is to reduce pain, control swelling, regain or maintain range of motion (ROM), and initiate quadriceps re-activation.29 In weeks 0-2 this may include the use of modalities such as ice for pain and swelling, stationary bike for ROM, and neuromuscular electrical stimulation to help with quadriceps re-activation. Strengthening exercises in this phase should focus on gaining active terminal knee extension with open chain exercises initially and then closed chain once they are tolerable and can be performed safely.30
In weeks 3-4, rehabilitation should be progressed to add weights to open chain strengthening, begin more functional closed chain strengthening, and complete proprioception drills, such as squats, leg press, and single leg stance. Flexion beyond 90 degrees with squatting activities should be avoided with grade III injuries in this phase.29 If the patient has full ROM with good strength and stability, they may progress to the final stage of rehabilitation at 5-6 weeks, as biological healing has created more knee stability.10
At the final stage of rehabilitation, the focus should shift to a progressive jog-to-run program and more traditional weight room activities, as well as early plyometrics. If cleared by the physician and strength is adequate at 6 weeks, lateral movements can slowly be introduced as long as knee stability is maintained. During this final stage of rehabilitation, the focus should be on higher-level strength activities and more functional sports-specific movements, such as single-leg hops, agility drills, and cutting movements.29
Operative Treatment of Medial Collateral Ligament Injuries
When nonoperative treatment fails to provide adequate stability, operative intervention is recommended.11,31 This lack of stability can be seen with valgus opening under stress loads most commonly at 30 degrees but also at 0 degrees of full extension during combined MCL + cruciate injuries. Additionally, in multiligamentous knee injuries involving disruption of the medial and posteromedial corner, in addition to the ACL, recommendations for acute sMCL +/- POL treatment have also been seen to minimize cruciate reconstruction failure, as well as facilitate early mobilization and rehabilitation.31
Repair vs. Reconstruction
The primary goal of surgical treatment of the medial knee structures, sMCL, dMCL, and POL, is to restore native anatomic relationships to achieve normal knee kinematics. In general, anatomic techniques are preferred secondary to their ability to restore native knee biomechanics, allowing early postoperative knee motion with improved outcomes and stability.32–35 Failure to reconstruct some ligaments during a staged procedure can result in nonphysiologic loading of reconstruction grafts. Therefore, for patients with multiligament injuries, single-stage procedures are favored when possible to minimize the risk of graft failure and to allow for early knee ROM.36 The complexity of medial knee anatomy and injury patterns has resulted in a multitude of reconstruction techniques. Primary repair is a treatment option that should be reserved for very select injuries, most notably acute avulsion injuries within the first 3 weeks following injury. In the pediatric population, repair may be considered for acute bony avulsions without midsubstance tearing or attenuation. For acute medial knee injuries that fail to improve with bracing and have valgus instability in flexion, augmented repair can be performed utilizing a semitendinosus autograft with suture anchor or socket fixation at the tibial and femoral attachments.33 For those medial injuries with instability in both flexion and full extension, anatomic MCL and posterior oblique ligament reconstruction is performed.26,37
Skeletally Immature Operative Techniques
MCL injuries in patients whose physes are open require great care to protect the potential of growth while stabilizing the knee.13,31 No single technique of MCL reconstruction or repair in a skeletally immature patient is universally accepted.13,31 Recommendations for near anatomic reconstruction derive from prior anatomic cadaver studies describing the location of the MCL and comparing this to the known location of the distal femoral and proximal tibial physes.11 Shea et al. looked closely at the location of the sMCL versus the knee physes and saw the proximal sMCL was found to be consistently distal to the distal femoral physis while the insertion of the distal sMCL was seen to be distal to the proximal tibial physis.11,13 This suggests an all-epiphyseal reconstruction at the femur but supports spanning the proximal tibial physis distally. While there is support for anatomic reconstruction as a preferred method of re-establishing stability to the medial side of the knee in skeletally mature patients, there is still a paucity of literature regarding ideal techniques as well as short, medium, and long-term outcomes in the setting of skeletal immaturity.13,31 One case report of sMCL repair with gracilis autograft reconstruction yielded good results at 6 months with no motion loss or recurrent instability and the patient returning to athletic activities at 6 months postoperatively; however, there was no reported follow-up after 6 months and no mention of assessment for growth disturbance.31
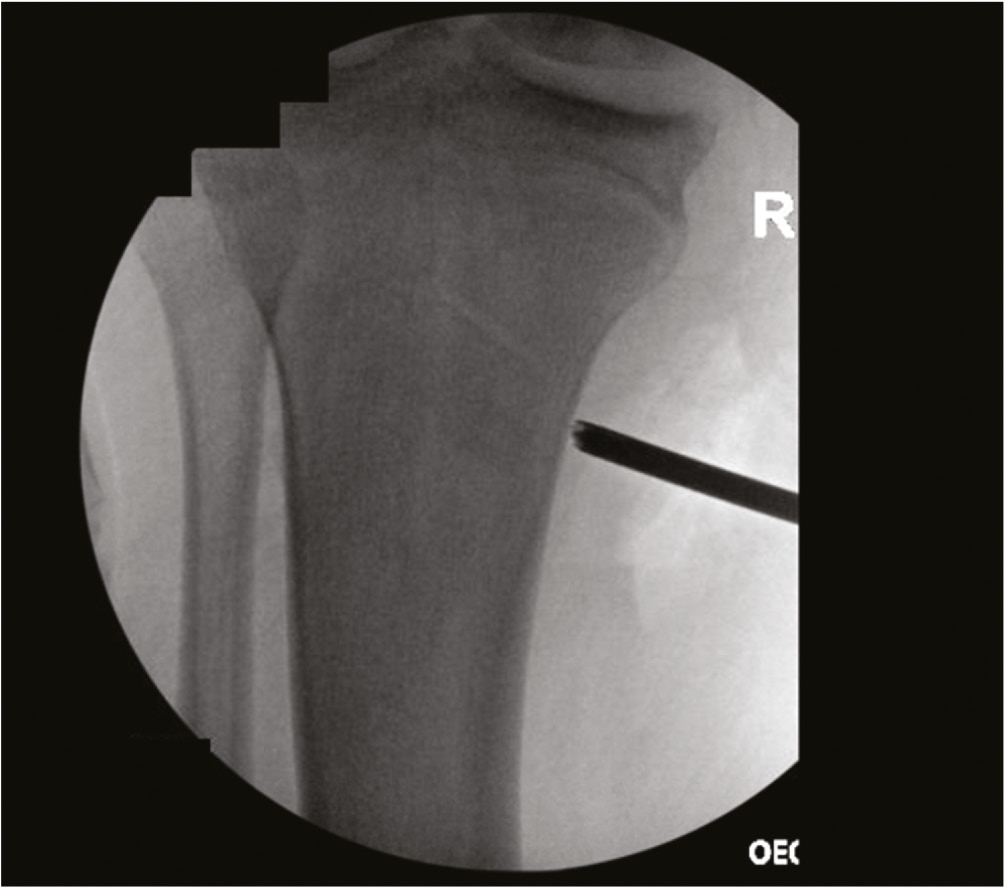
The authors preferred technique for MCL reconstruction in skeletally immature patients includes an all-epiphyseal femoral attachment at the origin of the sMCL near the medial epicondyle (Figure 11). Distally, spanning of the proximal tibial physis in order to attach the sMCL to its anatomic location is preferred (Figure 12). This distal attachment has been seen to be the primary stabilizer medially on cutting studies and therefore increases stability at the knee compared to staying all epiphyseal, which fails to reconstruct the distal limb of the sMCL.11 When the POL is also disrupted, such as in the setting of extensive multiligament knee injuries, MCL anatomic reconstruction with capsular imbrication (MARCI) technique is preferred to decrease tethering around the physis and due to a recent biomechanical analysis revealing better approximation of the intact state with imbrication in regards to valgus loading, internal and external rotation compared to the 4-tunnel anatomic reconstruction technique described by LaPrade.38
Figure 11. All-epiphyseal femoral attachment at sMCL proximal origin.
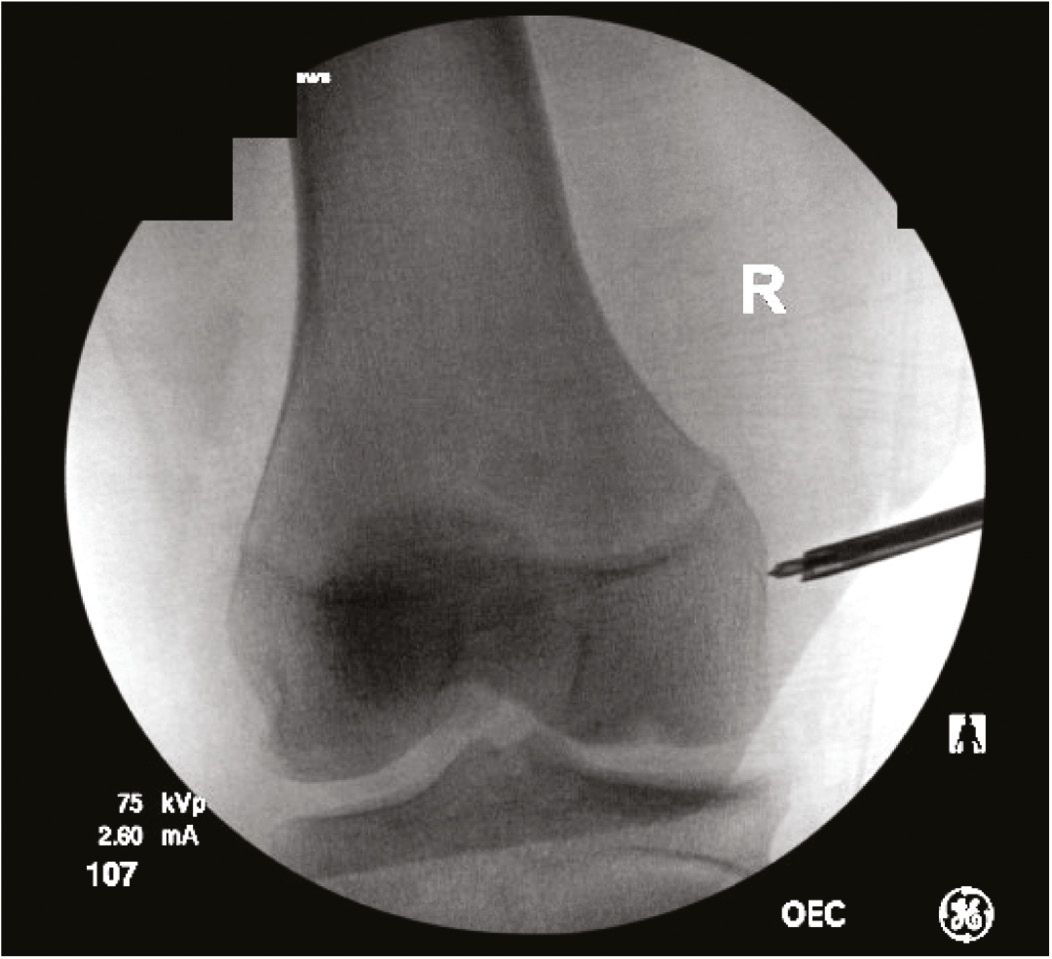
Figure 12. Distal sMCL insertion at proximal tibia.
Additionally, suture anchors with all-suture soft suture anchors are preferred for fixation of the MCL reconstruction to minimize tunnel convergence, especially in these routinely smaller knees.
Physical Therapy for Operative MCLs
Supervised, structured postoperative physical therapy is crucial to ensuring a successful return to prior functional levels of activities and sports in patients treated for their MCL injuries.
Early Postoperative Rehabilitation
Early postoperative rehabilitation goals include controlling pain and swelling, conserving ROM, regaining strength, and normalizing gait patterns.10,29 Reducing swelling is of utmost priority as prolonged knee effusions can inhibit strength gains secondary to quadriceps inhibition.10,19
Early ROM control can help prevent knee stiffness caused by adhesions and arthrofibrosis.10,39 A “safe zone,” often between 0-90 degrees, can be established during surgery and relayed from the surgeon to the rehabilitation team to be initiated during the first postoperative week.10,29,39 ROM progressions continue to vary from allowing 0-30 degrees in the first 2 postoperative weeks to remaining in full extension for 6 weeks.39,40 However, hyperextension and flexion greater than 90 degrees should be avoided, as these zones could tension and damage the graft or repair in the early phase.10 Patients should be progressed from passive ROM to active assisted ROM to active ROM, and effective exercises include the use of a stationary bike and heel slides. Additionally, manual therapy methods such as patellar mobilizations, soft tissue mobilizations, and scar mobilizations are effective.29,39
The patient should remain in a brace until ROM restrictions have been released (primarily around 4-6 weeks) and should be locked in extension for ambulation until quadriceps strength is sufficient as can be seen by a set of straight leg raises without quadriceps lag or when the surgeon feels it is safe to progress clinically.
Differing opinions exist on weight-bearing progression following operative treatment of the MCL, with some suggesting immediate postoperative weight-bearing and some suggesting delayed weight-bearing for up to 3-6 weeks postoperatively.10,29,40 Excessive tibial external and internal rotation as well as pivoting motions while the involved limb is planted should be avoided, as this could damage the graft.10 Therapists should monitor for an increase in edema or effusion during progressive weight-bearing.29 Once a patient can bear weight, emphasis should be placed on normalizing gait patterns.
Early strengthening can begin immediately and includes quadriceps sets and straight leg raises with the brace in place. Patients should begin with open chain exercises, focusing on dynamic knee stabilizers as well as lower extremity stabilizers above and below the knee.29,39 More progressive strengthening exercises can begin at weeks 4-8, which will include closed kinetic chain exercises. Double limb squatting and leg press can be utilized early, with range of motion limited between 0-70 degrees.10,39 Wijdicks et al. discuss that hamstring resistance or repeated hamstring exercises should be avoided for 4 months to prevent joint translation and graft stretching.10 Patients should be progressed from isometric to isotonic to eccentric exercise.39
Late Phase Rehabilitation
Late phase postoperative rehabilitation is identical to late phase nonoperative rehabilitation, including further functional strengthening, running, jumping, and sport-specific exercises. There is no consensus on when a patient should progress into running activities; however, it is well-accepted that this should be criterion-based versus time-based. Following a criterion-based protocol, return to running typically occurs around weeks 16-20.10,29,38,39 When progressing a patient’s program, requirements unique to their sport should be considered.
Outcomes
Recovery following medial knee injury is complex, and functional outcomes vary broadly due to heterogeneity in anatomy, treatment protocols, presence of concomitant injuries, and rehabilitation protocol.24 The sMCL can heal well nonoperatively with satisfactory long-term outcomes, as it is aided by robust vasculature.10 However, the probability of satisfactory long-term nonoperative outcomes decreases with the presence of concomitant ligamentous injuries and sustained valgus alignment.41
Nonoperative Treatment Outcomes
Isolated grade I and II MCL injuries can be managed nonoperatively through rehabilitation and functional bracing with good prognosis, including full return of strength and restored ROM and valgus stability.17 However, complete MCL injuries have better outcomes when treated operatively, as it has been shown patients with complete ligament disruption treated nonoperatively were more likely to have lower functional scores, increased instability, and a higher rate of osteoarthritis and valgus laxity on radiographs.24
Outcomes in Operative Treatment
Operative intervention is recommended when stability cannot be restored, particularly in chronic MCL tears or complete tears. Hughston and Barrett found that 94% of athletes with confirmed grade III MCL injuries and anteromedial rotatory instability treated operatively were able to return to their preinjury level of function.42 A later study on the same cohort of patients with an average of 22 years of follow-up demonstrated that 93% had sustained stability and normative range of motion.43
Both MCL reconstruction and repair have demonstrated improved patient-reported functional outcome scores at follow-up.44 However, the rates of postoperative knee stiffness and failure at a minimum 2-year follow-up were shown to be higher among patients who had a repair.44 In addition, range of motion deficits were more commonly reported in those who have MCL repair (between 0-50%) versus reconstruction (between 0-26.7%).44
A unique outcome more specific to skeletally immature patients is limb alignment and growth arrest. Aioki et al. present one case study of a skeletally immature athlete who had attempted nonoperative treatment that failed and went on to operative treatment with reconstruction and developed a significant genu valgum growth deformity requiring hemi-epiphysiodesis.45 This resultant deformity may have been due to overgrowth from the medial physis after surgical intervention or from undergrowth from the lateral physis after persistent valgus instability, causing increased lateral-sided loading and subsequent damage to the lateral aspect of the proximal tibial physis. Either way, this is an excellent example of the importance of continued alignment radiographs in the postoperative period to document normal growth.
Combined ACL + MCL Outcomes
There is mixed consensus regarding the ideal management for combined ACL/MCL injuries, particularly regarding the timing of the ACL reconstruction and its effect on functional outcomes. Animal models have demonstrated that the healing course of the MCL can be adversely affected by insufficiency of the ACL, supporting the idea that early ACL reconstruction may be more beneficial.46 In addition, Fetto and Marshall recommended early operative care of all combined ACL/MCL injuries, as a demonstrated 79% of mixed ACL/MCL lesions had very poor outcomes following nonoperative treatment protocols.17 In contrast, other studies have demonstrated significant improvements in functional outcomes with early rehabilitation and delayed reconstruction, particularly in the pediatric population. Sankar et al. described a retrospective cohort of patients who were treated with a hinged brace for their MCL injury followed by a delayed ACL reconstruction, and all patients met criteria for return to sport with improved Lysholm scores and full valgus stability at their last follow-up examination.5 Regardless of treatment protocol, restoration of the complex, multiplanar instability associated with concurrent compromise of multiple ligaments is central to achieving good outcomes.
Summary
While many MCL injuries in both skeletally mature and immature individuals can be treated successfully nonoperatively with bracing, physical therapy, and activity modifications, persistent laxity or multiligamentous injury may require operative intervention with reconstruction favored over repair in most cases. This is the first review article covering MCL injuries in pediatric and adolescent patients. More pediatric and adolescent-specific research regarding MCL injuries and treatments is needed to provide patients with improved guidance regarding their treatment and expectations for outcomes.
Acknowledgements
This manuscript was produced by pediatric orthopaedic sports medicine surgeons and physical therapists from the Pediatric Research in Sports Medicine (PRISM) Knee Ligament Research Interest Group (RIG).
Disclaimer
No funding was received. The authors report no conflicts of interest related to this manuscript.
References
- Lee RJ, Margalit A, Nduaguba A, et al. Risk factors for concomitant collateral ligament injuries in children and adolescents with anterior cruciate ligament tears. Orthop J Sports Med. 2018;6:2325967118810389.
- Kramer DE, Miller PE, Berrahou IK, et al. Collateral ligament knee injuries in pediatric and adolescent athletes. J Pediatr Orthop. 2020;40:71-77.
- Jarrett DY, Kramer DE, Laor T. Magnetic resonance imaging of medial collateral ligament avulsion fractures of the knee in children: a potentially underestimated injury. Pediatr Radiol. 2021;51:1705-1713.
- Tschauner S, Sorantin E, Singer G, et al. The origin points of the knee collateral ligaments: an MRI study on paediatric patients during growth. Knee Surg Sports Traumatol Arthrosc. 2016;24:18-25.
- Sankar WN, Wells L, Sennett BJ, et al. Combined anterior cruciate ligament and medial collateral ligament injuries in adolescents. J Pediatr Orthop. 2006;26:733-736.
- Majewski M, Habelt S, Steinbrück K. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184-188.
- Tadlock BA, Pierpoint LA, Covassin T, et al. Epidemiology of knee internal derangement injuries in United States high school girls’ lacrosse, 2008/09-2016/17 academic years. Res Sports Med. 2019;27(4):497-508.
- Shea KG, Grimm NL, Ewing CK, et al. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med. 2011;30(4):691-706.
- LaPrade RF, Engebretsen AH, Ly TV, et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000-2010.
- Wijdicks CA, Griffith CJ, Johansen S, et al. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92(5):1266-1280.
- Wijdicks CA, Ewart DT, Nuckley DJ, et al. Structural properties of the primary medial knee ligaments. Am J Sports Med. 2010;38(8):1638-1646.
- Wijdicks CA, Griffith CJ, LaPrade RF, et al. Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med. 2009;37(9):1771-1776.
- Shea KG, Cannamela PC, Dingel AB, et al. Anatomic dissection and CT Imaging of the anterior cruciate and medial collateral ligament footprint anatomy in skeletally immature cadaver knees. J Pediatr Orthop. 2020;40:e109-e114.
- Schmidt EC, Chin M, Aoyama JT, et al. Mechanical and microstructural properties of native pediatric posterior cruciate and collateral ligaments. Orthop J Sports Med. 2019;7:2325967118824400.
- Krych A, Odland A, Rose P, et al. Oncologic conditions that simulate common sports injuries. J Am Acad Orthop Surg. 2014;22:223-234.
- Dempewolf M, Kwan K, Sherman B, et al. Youth kicker’s knee: lateral distal femoral hemiphyseal arrest secondary to chronic repetitive microtrauma. J Am Acad Orthop Surg Glob Res Rev. 2019;3:e079.
- Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop. 1978;132(1):206-218.
- Corten K, Hoser C, Fink C, et al. Case reports: a Stener-like lesion of the medial collateral ligament of the knee. Clin Orthop Relat Res. 2010;468(1):289-293.
- Indelicato PA. Non-operative treatment of complete tears of the medial collateral ligament of the knee. JBJS. 1983;65(3):323-329.
- Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Relat Res. 1986;213:137-140.
- Frank C, Schachar N, Dittrich D. Natural history of healing in the repaired medial collateral ligament. J Orthop Res. 1983;1(2):179-188.
- Shrive N, Chimich D, Marchuk L, et al. Soft-tissue “flaws” are associated with the material properties of the healing rabbit medial collateral ligament. J Orthop Res. 1995;13(6):923-929.
- Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;226:103.
- Thornton GM, Johnson JC, Maser RV, et al. Strength of medial structures of the knee joint are decreased by isolated injury to the medial collateral ligament and subsequent joint immobilization. J Orthop Res. 2005;23(5):1191-1198.
- Reider B, Sathy MR, Talkington J, et al. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation: a five-year follow-up study. Am J Sports Med. 1994;22(4):470-477.
- Takakura Y, Matsui N, Yoshiya S, et al. Low-intensity pulsed ultrasound enhances early healing of medial collateral ligament injuries in rats. J Ultrasound Med. 2002;21(3):283-288.
- Demir H, Menku P, Kirnap M, et al. Comparison of the effects of laser, ultrasound, and combined laser + ultrasound treatments in experimental tendon healing. . Lasers Surg Med. 2004;35(1):84-89.
- Laprade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. 2012;42(3):221-233.
- Knee ligament sprain guidelines: revision 2017: using the evidence to guide physical therapist practice. J Orthop Sports Phys Ther. 2017;47(11):822-823.
- Moatshe G, Vap AR, Getgood A, et al. Medial-sided injuries in the multiple ligament knee injury. J Knee Surg. 2020;33(5):431-439.
- Gorin S, Paul DD, Wilkinson EJ. An anterior cruciate ligament and medial collateral ligament tear in a skeletally immature patient: a new technique to augment primary repair of the medial collateral ligament and an allograft reconstruction of the anterior cruciate ligament. Arthroscopy. 2003;19(10):E21-E26.
- LaPrade RF, Johansen S, Agel J, et al. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92:16-22.
- Wijdicks CA, Michalski MP, Rasmussen MT, et al. Superficial medial collateral ligament anatomic augmented repair versus anatomic reconstruction: an in vitro biomechanical analysis. Am J Sports Med. 2013;41:2858-2866.
- Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806-814.
- LaPrade RF, Spiridonov SI, Coobs BR, et al. Fibular collateral ligament anatomical reconstructions: a prospective outcomes study. Am J Sports Med. 2010;38:2005-2011.
- Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430-438.
- Coobs BR, Wijdicks CA, Armitage BM, et al. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med. 2010;38:339-347.
- Richter DL, McIver ND, Sapradit T, et al. A biomechanical comparison of the LaPrade technique versus a novel technique for reconstruction of medial-sided knee injuries. Am J Sports Med. 2022;50(8):2083-2092.
- Kim C, Chasse PM, Taylor DC. Return to play after medial collateral ligament injury. Clin Sports Med. 2016;35(4):679-696.
- D’Ambrosi R, Corona K, Guerra G, et al. Midterm outcomes, complications, and return to sports after medial collateral ligament and posterior oblique ligament reconstruction for medial knee instability: a systematic review. Orthop J Sports Med. 2021;9(11):23259671211056070.
- Phisitkul P, James SL, Wolf BR, et al. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77-90.
- Hughston JC, Barrett GR. Acute anteromedial rotatory instability. Long-term results of surgical repair. J Bone Joint Surg Am. 1983;65:145-153.
- Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow up. J Bone Joint Surg Am. 1994;76(9):1328-1344.
- Mowers C, Jackson GR, Condon JJ, et al. Medial collateral ligament reconstruction and repair show similar improvement in outcome scores, but repair shows higher rates of knee stiffness and failure: a systematic review. Arthroscopy. 2023;39(10):2231-2240.
- Hobson TE, Mortensen AJ, Metz AK, Aoki SK. Cozen’s phenomenon after repair of a medial collateral ligament periosteal avulsion in a pediatric athlete: a case report. JBJS Case Connect. 2021;11(4). doi: 10.2106/JBJS.CC.21.00481.
- Woo SL, Young EP, Ohland KH, et al. The effects of transaction of the anterior cruciate ligament on the healing of the medial collateral ligament. A biomechanical study of the knee in dogs. J Bone Joint Surg Am. 1990;72:382-339.
